Introduction
Systemic arterial hypertension (SAH) is a chronic, multifactorial, non-communicable disease considered the leading risk factor for other cardiovascular diseases and one of the leading causes of death worldwide. 1-3 In older adults, SAH is particularly prevalent due to various factors, including the natural aging of the cardiovascular system, such as arterial stiffness and the accumulation of atheromatous plaques over time. 4,5 Adequate control is essential to prevent complications, so it is important to follow medical advice regarding the proper use of medications. 5,6
It is important to consider drug interactions, especially in older adults who often use multiple medications for various health conditions, to avoid harmful interactions3. Older adults are more susceptible to medication side effects, such as falls, dizziness, and balance disturbances. Some patients report feeling dizzy or fearful of falling when using antihypertensive drugs, especially when getting up quickly. 7-9
Understanding specific risk factors for falls in older hypertensive individuals can help identify areas where preventive interventions may be most effective. This is important for developing targeted and personalized fall prevention strategies for this vulnerable population. Thus, this study aimed to investigate the associations between antihypertensive medication use and the risk and fear of falling in hypertensive older adults.
Methods
This study employed a quantitative, observational, and cross-sectional design, adhering to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines. It was approved by the Research Ethics Committee of Cesumar University (UniCesumar) under protocol No. 6.301.362.
Participants
A non-probabilistic, intentional, and convenience-based sampling approach was used to select 70 independent community-dwelling older adults (aged 60 years or older) of both genders, all diagnosed with systemic arterial hypertension (SAH) and undergoing treatment at a Medical Specialties Center in the municipality of Sapezal, Mato Grosso, Brazil. The diagnosis of SAH and antihypertensive medication use were confirmed through electronic health records at the healthcare facility.
Participants were excluded if they:
- Used benzodiazepines, due to their mild nervous system inhibition, which includes anticonvulsant, sedative, muscle relaxant, and tranquilizing effects.
- Had osteoarticular diseases or injuries that prevented them from performing the required physical tests.
- Presented cognitive impairments that hindered accurate completion of the questionnaires.
- Had clinical evidence of pre-renal or post-renal hepatic or thyroid dysfunction.
Instruments
The authors developed a semi-structured questionnaire to assess the sociodemographic and health profiles of the older participants. The questionnaire included items on age, age group, sex, income in minimum wages, occupational status, retirement, education level, marital status, use of antihypertensive medication, use of medications in general, presence of comorbidities, history of falls and history of near falls.
Fall risk was assessed using the Timed Up and Go (TUG) test, a widely used tool to evaluate functional mobility and fall risk in older adults. In this test, participants rose from a chair, walked three meters, turned around, and returned to the chair. Individuals underwent assessment only after familiarization with the task. A predictive value of ≥ 12.47 seconds indicated high fall risk, while ≤ 12.47 seconds indicated low fall risk. 10
Fear of falling was evaluated using the Falls Efficacy Scale-International (FES-I), a validated questionnaire designed to assess fear of falling in daily activities. It consists of 16 items covering different daily tasks, with responses ranging from 1 (not at all concerned) to 4 (extremely concerned). The total score ranges from 16 to 64, with higher scores indicating greater fear of falling. Cutoff points were used to categorize participants: < 23 - no fear of falling; ≥ 23 - occasional fear of falling; ≥ 31 - recurrent fear of falling. 11
Procedures
Permission for the study was obtained from the Municipal Health Regulation Center of Sapezal-MT. The center arranged appointments for specialized consultations in Cardiology and Orthopedics, allowing patients to be referred to the Medical Specialties Center for consultations scheduled in advance. This facilitated contact with older individuals diagnosed with (or without) SAH and access to their medical records.
Eligible participants were identified through their scheduled consultations and invited to participate in the study. Those who met the inclusion criteria and agreed to participate signed an informed consent form (ICF), after which data collection was conducted by the researcher between September and November 2023.
Data análisis
Data analysis was performed using SPSS software version 25.0. Descriptive and inferential statistics were applied. Frequency and percentage were used as descriptive measures for categorical variables. The Chi-square test compared proportions of fall risk and fear of falling with time since SAH diagnosis, duration of antihypertensive use, and number of antihypertensive drugs used. Binary Logistic Regression (both crude and adjusted analyses) examined associations of SAH diagnosis, duration of antihypertensive use, and number of antihypertensive medications used (independent variables) with presence of fall risk and fear of falling associated with recurrent falls (dependent variables). Only variables showing significance levels of p ≤ 0.05 in the Chi-square test for association with fall risk and fear of falling were included in the regression analysis. Model fit was assessed using the Hosmer-Lemeshow test. A significance level of p < 0.05 was considered.
Results
Among the 70 older hypertensive individuals, a predominance of women was observed (67.1 %), aged between 60 and 70 years (64.3 %), without a partner (58.6 %), with a monthly income ranging from more than one to two minimum wages (64.3 %), retired (77.1 %), and inactive in occupational status (85.7 %). A majority reported regular health perception (67.1 %), regularly used three to four medications (71.4 %), and had no history of falls in the last six months (61.4 %). Most older individuals use two or more antihypertensive medications regularly (72.9 %), were diagnosed with SAH within the last five years (65.7 %) and have been using antihypertensive medications for at least one year (70.0 %).
The majority of older hypertensive individuals showed a presence of fall risk (71.4 %) and fear of falling associated with recurrent falls (60.0 %). A significant difference was found between groups regarding the number of antihypertensive medications (p < 0.001) and duration of antihypertensive use (p = 0.012), highlighting a higher proportion of older individuals using two or more antihypertensive medications and having had SAH diagnosed for more than four years, who also showed fall risk.
A significant difference was found between groups regarding the number of antihypertensive medications (p < 0.001), duration of antihypertensive use (p = 0.012), and time since SAH diagnosis (p = 0.004), indicating a higher proportion of older individuals using two or more antihypertensive medications, diagnosed with SAH for more than five years, and using antihypertensive medications for more than four years, who also reported fear of falling associated with recurrent falls.
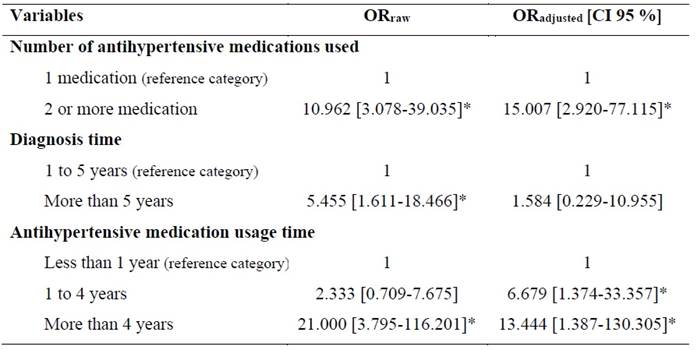
For logistic regression analysis modeling, only variables with a significance level < 0.20 in the Chi-square test for the presence of fall risk and fear of falling (Tables 1 and 2) were considered. Table 1 presents the factors associated with fall risk. In the crude analysis, the following factors individually showed significant association with the presence of fall risk: number of antihypertensive medications (p < 0.001) and duration of antihypertensive use (p = 0.047). When the analysis was adjusted for all variables in the model, only the number of antihypertensive medications remained significantly associated (p < 0.05) with the presence of fall risk. It is noteworthy that older individuals using two or more antihypertensive medications have a 48.167 (95 % CI = 5.361-432.771) times higher chance of experiencing fall risk compared to those using only one antihypertensive medication.
Table 1: Factors associated with the presence of risk of falls in older individuals. Sapezal, Brazil, 2023.
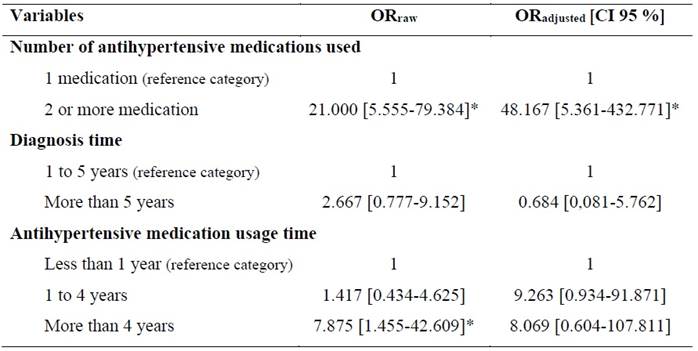
*Significant association - p < 0.05: binary logistic regression. Alternatively, adjusted for all variables of the model. OR: Odds Ratio; CI: Confidence Interval.
Table 2 presents the factors associated with fear of falling and recurrent falls. In the crude analysis, all variables individually showed significant association with the presence of fear of falling associated with recurrent falls (p < 0.05). When the analysis was adjusted for all variables in the model, only the number of antihypertensive medications and duration of antihypertensive use remained significantly associated (p < 0.05) with fear of falling associated with recurrent falls. It is noteworthy that older individuals using two or more medications have a 15.007 (95 % CI = 2.920-77.115) times higher chance of experiencing fear of falling associated with recurrent falls compared to those using only one antihypertensive medication. Additionally, older individuals using antihypertensive medications for between one to four years and more than four years have, respectively, 6.679 (95 % CI = 1.374-33.357) and 13.444 (95 % CI = 1.387-130.305) times higher chances of experiencing fear of falling associated with recurrent falls compared to those using antihypertensive medications for less than one year.
Discussion
We found that older hypertensive individuals using two or more antihypertensive medications have a higher likelihood of experiencing fall risk and greater fear of falling compared to those using only one antihypertensive. Gomes et al. 12 emphasize that the use of multiple medications is associated with a higher risk of side effects and drug interactions. Antihypertensive medications, in particular, can cause symptoms such as dizziness, weakness, blurred vision, and fainting, especially when used in combination. 13 Moreover, the use of multiple antihypertensive medications can result in excessive blood pressure reduction, leading to orthostatic hypotension. 14 Orthostatic hypotension is associated with an increased risk of falls, as it can cause dizziness and fainting in older adults. 15
We also found that older hypertensive individuals who have been using antihypertensives for more than a year are more likely to experience fear of falling associated with recurrent falls compared to those using antihypertensives for less than a year. This likelihood is even higher for those who have been using antihypertensives for more than four years. This may be because prolonged use of antihypertensive medications is associated with a greater risk of developing side effects and complications from the treatment. These side effects can include dizziness, muscle weakness, imbalance, and orthostatic hypotension, which increase the risk of falls. 16 Older individuals who have been using antihypertensives for a longer period may have an increased perception of vulnerability due to these cognitive and sensory changes, contributing to a greater fear of falling. 17
A higher proportion of older individuals with a longer duration of SAH diagnosis was found to have a risk of falls and fear of falling associated with recurrent falls. First, according to Fuchs and Whelton, 1 SAH is a chronic condition that can cause progressive damage to blood vessels, the heart, the brain, and other organs over time. This damage can result in health complications affecting cardiovascular function, brain health, and balance and motor coordination, thus increasing the risk of falls. 18,19
Another aspect is the psychological impact of living with SAH for an extended period. Older individuals who have had chronic conditions for years may develop persistent concerns about their health and well-being, particularly if they have experienced complications related to SAH in the past, such as severe cardiovascular events. 20 Additionally, the prolonged time since the diagnosis of SAH may be associated with a gradual deterioration in overall health and physical functionality. Older individuals may experience progressive declines in muscle strength, balance, and coordination, heightening their vulnerability to falls and, consequently, their fear of falling. 21
The study's limitations include selection bias from a non-probabilistic sample, restricting generalizability, and potential information bias from self-reported fall risk and fear data. Unmeasured variables, like health conditions and physical activity, may confound results. The cross-sectional design prevents causal analysis, and findings might be context specific. Another important limitation of this study was the small sample size (N = 70), which may have affected the precision of the statistical estimates. Smaller samples tend to produce wider confidence intervals, indicating greater uncertainty in the odds ratio estimates. This occurs because the limited number of observations reduces the stability of statistical calculations, increasing the variability of the results. Moreover, with a reduced number of participants, detecting statistically significant associations becomes more challenging, particularly when the effects under investigation are subtle or moderate. Expanding the sample size in future studies could provide more robust and precise estimates, reducing uncertainty and improving the generalizability of the findings.
Conclusion
Our findings indicate a significant link between the use of multiple antihypertensive medications and a higher risk of falls, as well as increased fear of falling in older hypertensive adults. Specifically, those using two or more medications are more likely to experience these risks compared to those using a single medication. Additionally, the duration of medication use is associated with fear of falling, as older adults on these drugs for over a year tend to have more recurrent falls, underscoring the need to consider both the quantity and duration of medication.
These findings have important clinical implications, as they highlight the necessity for comprehensive medication reviews in older hypertensive adults to balance blood pressure management with fall prevention strategies. Healthcare providers should assess medication regimens regularly, consider deprescribing strategies when appropriate, and incorporate fall risk assessments into routine care.
Future research should explore longitudinal studies to establish causal relationships and investigate alternative treatment approaches that minimize fall risk while maintaining effective blood pressure control. Additionally, intervention studies focusing on fall prevention programs tailored for hypertensive older adults could provide valuable insights into mitigating these risks.