Services on Demand
Journal
Article
Related links
Share
Odontoestomatología
Print version ISSN 0797-0374On-line version ISSN 1688-9339
Odontoestomatología vol.26 no.43 Montevideo 2024 Epub June 01, 2024
https://doi.org/10.22592/ode2024n43e331
Update
Application of cryotherapy in endodontics: its importance in pain control
2Departamento de Biología Odontológica, subunidad Fisiología general y buco-dental Facultad de Odontología, Universidad de la Repúblicaerotemb@yahoo.com.ar
Introduction:
Endodontics is the dental discipline that deals with the morphology, physiology and pathology of the dental pulp and periradicular tissue. It includes the etiology, prevention, diagnosis and treatment of pulp disorders, as well as its repercussions in the periapical region and the rest of the organism. The purpose is to relieve pain and preserve the teeth in function. Pain originating from teeth or surrounding tissues is one of the main reasons for dental consultation.
Specific objectives:
to analyze its physiological mechanism of action; the efficacy in reducing pain in endodontic therapies with different initial diagnoses; describe its forms of clinical application; establish the contraindications or possible inconveniences that its application may present.
Methodology:
The work is a narrative review. The bibliographic search was carried out with the following MeSH (Medical Subject Heading) terms: cryotherapy, endodontic, intracanal irrigation, dental pain and their corresponding descriptors in DeCS health sciences: cryotherapy, endodontics, intracanal irrigation and dental pain. The inclusion criteria were: articles available in full text that contain at least one keyword in the title and/or abstract, in English, Spanish or Portuguese, with no time limit. Articles with studies in animals or in deciduous teeth were excluded.
Conclusions:
According to the present work, there are scientific studies that positively support the application of cryotherapy for pain control in endodontics.
Keywords: endodontics; cryotherapy; intracanal irrigation; dental pain
Introducción:
La endodoncia es la disciplina odontológica que estudia la morfología, fisiología y patología de la pulpa dentaria y del tejido perirradicular. Comprende la etiología, prevención, diagnóstico y tratamiento de las alteraciones pulpares, así como sus repercusiones en la región periapical y el resto del organismo. Su finalidad es aliviar el dolor y preservar las piezas dentales en función dentro del sistema estomatognático. El dolor que se origina en piezas dentarias o tejidos circundantes es uno de los principales motivos de consulta odontológica.
Objetivos específicos:
analizar su mecanismo fisiológico de acción; la eficacia en la reducción del dolor en las terapias endodónticas con diferentes diagnósticos iniciales; describir sus formas de aplicación clínica; establecer las contraindicaciones o los posibles inconvenientes que pueda presentar su aplicación.
Metodología:
El trabajo es una revisión narrativa. Se realizó la búsqueda bibliográfica con los siguientes términos MeSH (Medical Subject Heading): cryotherapy, endodontic, intracanal irrigation, dental pain y sus correspondientes descriptores en ciencias de la salud DeCS: crioterapia, endodoncia, irrigación intracanal y dolor dental. Los criterios de inclusión fueron: artículos disponibles a texto completo que contengan al menos una palabra clave en título y/o resumen, en idioma inglés, español o portugués, sin límite temporal. Se excluyeron los artículos con estudios en animales o en piezas dentarias deciduas.
Conclusiones:
De acuerdo al presente trabajo existen estudios científicos que sostienen positivamente la aplicación de la crioterapia para el control del dolor en endodoncia.
Palabras claves: endodoncia; crioterapia; irrigación intracanal; dolor dental
Introdução:
Endodontia é a disciplina odontológica que trata da morfologia, fisiologia e patologia da polpa dentária e do tecido perirradicular. Inclui a etiologia, prevenção, diagnóstica e tratamento das desordens pulpares, bem como suas repercussões na região periapical e no restante do organismo. O objetivo é aliviar a dor e preservar os dentes em função. A dor originada nos dentes ou tecidos circundantes é um dos principais motivos de consulta odontológica.
Objetivos específicos:
analisar seu mecanismo fisiológico de ação; a eficácia na redução da dor em terapias endodônticas com diferentes diagnósticos iniciais; descrever suas formas de aplicação clínica; estabelecer as contraindicações ou possíveis inconvenientes que a sua aplicação possa apresentar.
Metodologia:
O trabalho é uma revisão narrativa. A busca bibliográfica foi realizada com os seguintes termos MeSH (Medical Subject Heading): crioterapia, endodontia, irrigação intracanal, dor dentária e seus correspondentes descritores no DeCS ciências da saúde: crioterapia, endodontia, irrigação intracanal e dor dentária. Os critérios de inclusão foram: artigos disponíveis em texto completo que contenham pelo menos uma palavra-chave no título e/ou resumo, nos idiomas inglês, espanhol ou português, sem limite de tempo. Foram excluídos artigos com estudos em animais ou em dentes decíduos.
Conclusões:
De acordo com o presente trabalho, existem estudos científicos que apoiam positivamente a aplicação da crioterapia para controle da dor em endodontia.
Palavras-chave: endodontia; crioterapia; irrigação intracanal; dor de dente
Introduction
Endodontics is the branch of dentistry that studies dental pulp diseases and those affecting teeth with necrotic pulp, whether with or without periapical complications 1. It encompasses the etiology, diagnosis, prevention, and treatment of dental pulp diseases and their complications 2. Most often, these conditions are pulpal or periapical inflammatory states, with dental caries being the predominant etiological factor (3.
The term cryotherapy derives from the Greek cryos meaning cold, and therapeia, indicating cure 4; that is, lowering tissue temperature for therapeutic purposes, not by implementing cold but rather by extracting heat 5. Local cooling of a body area is achieved by transferring body heat to an external element whose temperature is much lower. Heat exchange occurs through various physical mechanisms: conduction, convection, and evaporation 6.
A common fear among patients undergoing endodontic treatment is the possibility of experiencing pain. Pain is defined as "an unpleasant sensory and emotional experience associated with or similar to that associated with actual or potential tissue injury" 7.
In recent times, cryotherapy has gained popularity as a technique to alleviate postoperative pain. When utilized in surgery, it is referred to as cryosurgery. In dentistry, cryotherapy is employed following extractions, periodontal and implant surgeries to mitigate pain 8. Cryoanesthesia, a form of topical anesthesia, is utilized to alleviate pain in the skin and mucous membranes through cooling without inducing freezing. It can be employed in some dental procedures 9.
Pain following endodontic treatment can be highly frustrating for both the patient and the dentist. Typically, patients assess pain and post-appointment swelling as indicators of the practitioner's expertise. Such patient experiences and misconceptions underscore the significance of minimizing postoperative endodontic pain 10.
Methodology
This work is a narrative review. A comprehensive literature search was conducted using the following MeSH (Medical Subject Heading) terms: cryotherapy, endodontic, intracanal irrigation, dental pain, along with their corresponding descriptors in DeCS health sciences: crioterapia, endodoncia, irrigación intracanal, and dolor dental.
Inclusion criteria comprised articles available in full-text containing at least one keyword in the title and/or abstract, in English, Spanish, or Portuguese, with no temporal constraints.
Exclusion criteria comprised studies conducted on animals or deciduous teeth.
The search was enhanced by a manual examination of references cited in the selected articles. Both primary and secondary sources of information were consulted. The search period extended from May 2021 to May 2023. An electronic bibliographic review of the literature was conducted across the Bireme (bvs) and PubMed databases, combining keywords such as Endodontic, Cryotherapy, Intracanal irrigation, Dental pain, and their equivalents in Spanish and Portuguese.
Background
In 3000 BC, the Egyptians were the first to apply cryotherapy to reduce inflammation and treat injuries. In ancient Greece, Hippocrates recommended the local or systemic application of cold for therapeutic purposes on injured individuals in 400 BC 10,11. However, it was James Arnott in 1851 who first reported and demonstrated the use of freezing therapy to treat a malignant disease using a mixture of salt and ice (4.
Cryotherapy has been utilized for many years in managing pain and facilitating postoperative recovery in sports injuries and surgical procedures. It has demonstrated effectiveness in reducing edema, pain, swelling, and recovery time with short-term applications in orthopedic, abdominal, gynecological, and hernia surgeries 12. Cryotherapy is defined as the therapeutic application of any substance to the body that removes heat, resulting in a decrease in tissue temperature 13.
In dentistry, it is commonly employed after intraoral surgical procedures to control postoperative pain 12. It is effective in treating various soft tissue lesions of the oral cavity, including keratotic, hyperplastic, granulomatous, vascular, pigmented, and salivary gland lesions. It has a significant advantage over other treatment modalities: it leaves minimal or no scarring. It is highly beneficial for treating mucous cysts of the floor of the mouth due to their minimal tendency to recur 14.
Development
Symptomatic apical periodontitis is the typical manifestation of postendodontic pain. It entails an acute inflammatory reaction akin to that observed in other connective tissues of the body, characterized by vasodilation, increased vascular permeability, and leukocyte migration from blood vessels to the site of tissue injury. Inflammatory mediators regulate this process, resulting in tissue damage, pain, and swelling. Cryotherapy has three fundamental effects: on vascular, neurological, and tissue metabolism 14.
At the vascular level, it induces vasoconstriction and slows down metabolism by decreasing biochemical reactions, thereby limiting oxygen demand at the cellular level and reducing the formation of free radicals in the tissues (15. Consequently, the amount of fluid leakage at the periradicular level as exudate decreases, resulting in reduced edema and swelling following biomechanical preparation 4. The most significant vasoconstriction occurs at a temperature of 15°C (15. At the neurological level, the application of cold induces analgesia in nociceptive nerve fibers by reducing conduction velocity. This effect differs between myelinated A-δ (A delta) nerve fibers and unmyelinated C nerve fibers; the former are completely deactivated at 7°C, while the latter are deactivated at 3°C. Additionally, it stimulates the secretion of endorphins, which bind to receptors in the dorsal horn of the spinal cord, inhibiting nociceptive transmission to the central nervous system. Another consequence of cryotherapy is the inhibition of tissue nociceptors, resulting in a local anesthetic effect known as cold neuropraxia 16. At the level of tissue metabolism, there is a decrease in the speed of biochemical reactions, leading to reduced formation of free radicals in the tissues, lower oxygen consumption, prevention of hypoxia and other cellular lesions (4.
In the oral and dental field, nociceptive stimuli on the pulp and/or periodontal tissue lead to the release of chemical mediators from two sources: bradykinin from plasma and prostaglandin E2 (PGE2) from damaged cells. Both act on trigeminal free nerve endings, with PGE2 sensitizing them and bradykinin completing the excitation, resulting in action potentials in afferent nerve fibers that convey pain to the central nervous system (CNS) (17.
Pain control in endodontic therapy requires good management in daily practice, given its potential to cause patient dissatisfaction and impact their quality of life. The incidence of pain in endodontic treatment ranges from 3 to 58%, and at the end, it may be due to mechanical and chemical lesions, along with the presence of microorganisms in the periapical region 18. Several strategies for pain and inflammation control include occlusal reduction, long-term anesthesia administration 19, psychological treatment 20, and the use of various mechanical techniques during canal procedures 8. Moreover, the use of non-steroidal anti-inflammatory drugs such as paracetamol or corticosteroids, though the second option poses side effects such as renal and hepatic disorders, gastrointestinal intolerance, and even asthma. In order to avoid these inconveniences, alternative treatments such as lymphatic drainage, laser, cryotherapy (16 and phototherapy (21 are suggested.
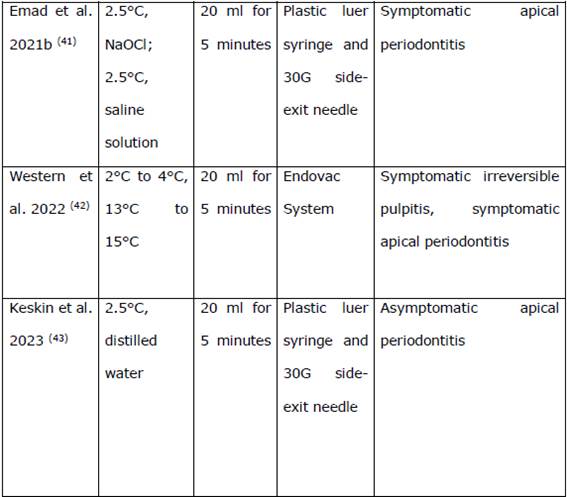
Vera et al., 2015 introduced cryotherapy in endodontics. In an ex vivo study on 20 freshly extracted human uniradicular teeth, they observed a significant reduction in the external temperature of the apical 4 mm of the root by 10°C. This reduction persisted for at least 4 minutes after continuous irrigation with 20 ml of cold saline at 2.5°C for 5 minutes using the Endo Vac (Endodontic Vacuum) system 5. It is a negative pressure irrigation procedure that involves an irrigation/evacuation tip connected to a syringe containing the irrigant and to the suction system of the dental unit, along with a small device where the microcannula and macrocannula are placed. The microcannula can be utilized at the working length in canals instrumented to a minimum caliber of #35 within a specific timeframe 22. Since then, numerous clinical and in vitro studies have been conducted on the application of intracanal cryotherapy (see Table 1), primarily focusing on the reduction of postendodontic pain, with a consistent decrease reported by various authors.
There is no consensus on the duration required for a therapeutic effect of cryotherapy. However, physiotherapy studies by Grant showed that treating 7000 ambulatory patients with ice therapy for between 5 and 7 minutes is adequate to induce muscle numbness. Waylonis reported evidence of superficial anesthesia after massaging the legs with ice for 4.5 minutes. Mc Gown demonstrated changes in inflamed quadriceps muscle tissue following a 5-minute ice massage 5. At the dental level, there are differences in the transmission of cold to the periodontal ligament in the apical and coronal portions of the tooth due to differences in dentin width and mineralization in these areas. The root of the cervical third contains more dentinal tubules with larger diameters, while the apical third is denser and more mineralized. Apical sclerotic dentin is less permeable than coronal dentin 5. Uniradicular teeth in the apical third typically present 1 to 7 pulp ramifications, which enhance cold transmission compared to multirooted teeth 23. Another question pertains to the temperature at which cellular death occurs, which seemingly does not occur at temperatures above -20°C, although most tissues freeze at -2.2°C (5. The reduction in blood flow and cellular metabolism induced by cryotherapy triggers an anti-edema effect, thereby contributing to analgesia 24.
Contraindications:
Cryotherapy is contraindicated in individuals with Raynaud's disease due to its impact on the smaller blood vessels that supply blood to the extremities, leading to excessive vasoconstriction that compromises irrigation to the affected area. Similarly, individuals with hypersensitivity to cold may experience symptoms such as redness, urticaria, severe pain, and muscle spasms (24. Moreover, it is contraindicated in individuals with cold intolerance, cryoglobulinemia, paroxysmal hemoglobinuria, peripheral nerve regeneration, peripheral vascular disease, or hypoesthetic areas. Freezing temperatures typically range between -4°C and -10°C; therefore, a safety margin around 15°C should be maintained 5. In patients with cardiac conditions such as arrhythmias, angina pectoris, and hypertension, the use of cryotherapy is controversial due to the potential increase in blood pressure resulting from vasoconstriction 24.
Discussion:
Endodontic treatment provides a favorable environment in the periradicular region for healing by thoroughly removing tissue debris and minimizing the presence of microorganisms in the root canal system, followed by complete obturation in all three dimensions (3D) of the shaped root canal space 37,39. However, the treatment process itself can induce pain. Various strategies, including cryotherapy, the latest advancement in endodontics, are suggested to mitigate this issue 37. Cryotherapies involving ice, cold water, and cold air have gained popularity due to their ability to remove heat, lower tissue temperature, and modify blood flow in humans 44. Postoperative pain is one of the major problems in endodontic treatment, even when proper treatment steps are followed 45. Teeth with periapical pathology are at greater risk of developing pain, and symptomatic teeth are more likely to have pain regardless of the condition of the dental pulp 29. Postoperative pain is the result of a complex multifactorial process influenced by factors inherent to the patient, the tooth undergoing treatment, the intervening operator 16, as well as inflammatory chemical mediators, cyclic nucleotide changes, modifications in local adaptation, and periapical tissue pressure 36. Periradicular inflammation arises from mechanical, microbial, and/or chemical injury to the periapical tissues. Even when not forced through the apical foramen, filling materials provoke an inflammatory reaction 12. Cold saline solutions used as final irrigations have been proven to reduce the external root surface temperature by over 10°C, maintaining it for 4 minutes 5. This decrease in external root surface temperature limits inflammatory reactions, the production and release of algesic substances, and the edema in the periapical region. Cryotherapy slows down peripheral nerve conduction, gradually reducing the speed of nerve fiber conduction until it halts completely. Concerning dental pulp, complete deactivation of A-δ fibers and partial deactivation of C fibers occur around 3°C 37. Ernst and Fialka observed that moderate cold application could not diminish nerve conduction in C fibers. It also activates thermal receptors that reduce the transmission of painful stimuli (12. Among the advantages of cryotherapy, its ease of application stands out, as it does not require any additional attachments - while it can be applied more effectively with the Endo Vac system, it is not a necessary requirement. This was demonstrated by Sadaf et al. in their meta-analysis comparing the use of Endo Vac to a syringe with a needle, where they concluded that there are no significant differences in using these instruments for cryotherapy application 46. Endovac is linked to a lower risk of extrusion of the irrigation agent and apical detritus into periapical tissues and maxillary sinuses 24.
Sodium hypochlorite (NaOCl) is the most widely employed irrigant in endodontics due to its extensive antimicrobial activity and ability to dissolve organic matter. However, it is irritating to periapical tissues, particularly at high concentrations. The concentration of NaOCl varied among studies; in Yadav's research, it was substituted with Herbal Triphala to prevent potential irritation, along with EDTA 32. The absence of a standardized cryotherapy protocol results in a lack of uniformity regarding the type, volume, and temperature of the irrigation agent used. Among the studies presented, saline was the most commonly utilized irrigation solution for cryotherapy, followed by EDTA combined with saline. The volume and temperature varied, ranging from 5 to 20 ml and from 1°C to 15°C.
While the protocols employed in the studies vary significantly, the majority of them reported lower rates of postoperative pain in cryotherapy groups compared to control groups, regardless of the agent, volume, or temperature used. Therefore, the type of irrigant agent may be considered less important than maintaining low temperatures, which promote local analgesia and reduce the likelihood of postoperative pain (47. Both Gundogdu 10 and Yadav (31) conducted studies utilizing intraoral and extraoral cryotherapy in the same way. The only difference was in the wrapping material used for the piece of ice in the extraoral application; Gundogdu used paper instead of gauze. In both cases, a significant reduction in postoperative pain was observed compared to the control group, as well as with intracanal application. Thus, despite being more uncomfortable for the patient, it could be considered as an alternative application method to take into account 31. One of the primary problems regarding intracanal cryotherapy, as indicated by the in vitro studies conducted by Keskin 31 and Jain 38, is the reduction in tooth fracture resistance. Despite both studies utilizing the same volume, duration, and irrigation temperature of 2.5°C, Western's investigation deviated from the commonly used temperature range of 2 to 4°C to a higher range of 13 to 15°C and still achieved a comparable reduction in pain. Therefore, further in vitro or clinical studies employing this temperature range are necessary to assess the long-term effects on tooth strength (42.
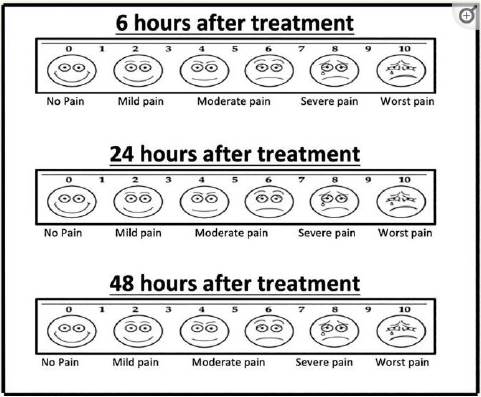
Patients can assess their pain levels using a Visual Analog Scale (VAS) questionnaire, categorizing pain as follows: 0 for no pain; 1-3 for mild pain; 4-6 for moderate pain; 7-9 for severe pain; and 10 for the worst pain 29. (Fig. 1)
In Jaiswall's study 34, pain scores were low in the cryotherapy group, despite a reduced intake of analgesics, suggesting the potential simultaneous use of these two methods (24. A systematic review and meta-analysis conducted by Smith et al. regarding NSAIDs for post-endodontic pain management concluded that ibuprofen is an effective analgesic for controlling post-endodontic pain 29. Furthermore, Di Spirito's study of systematic review recommends ibuprofen 600 mg alone or combined with paracetamol 1000 mg as the first-choice treatment 21. Studies by Vieyra, Alharthi, Akpinar, Jaiswall, and Western underscore that cryotherapy diminishes post-endodontic pain and the necessity for analgesic medication, with no statistically significant differences observed among the procedures employed 29,30, 34,40,42. Cryotherapy alleviates pain associated with both symptomatic irreversible pulpitis and symptomatic apical periodontitis (48. In these cases, its effect may be greater as inflammation is not confined within the root canal. This can be explained by the cold saline solution's effect on reducing edema and inflammation, acting as an anti-inflammatory in the periapical area 26. Emad's studies 41 elucidate the mechanism of action of cryotherapy concerning inflammatory markers known as cytokines. Comparative results of cryotherapy application against control groups reveal reduced levels of proinflammatory cytokines IL-1β and IL-6, alongside elevated levels of the anti-inflammatory cytokine IL-10. A recent study by Keskin also demonstrated a reduction in cytokines IL-1β, IL-6, and IL-2 43. Interleukins 1β, IL-6, and IL-10 have been widely studied for their role in the pathophysiology of periradicular disease. Moreover, they are considered the most important in human osteoclastic activity, with their presence correlating to the size of periapical lesions. Strict counteraction of proinflammatory pathways is essential to prevent unnecessary tissue damage. There is a balance between proinflammatory and anti-inflammatory cytokines in chronic inflammatory processes regulating the degree of host response to antigen stimulation 23.
Conclusions:
Based on this narrative review, there is scientific evidence supporting the application of cryotherapy for pain management in endodontics, particularly in cases of symptomatic irreversible pulpitis and symptomatic apical periodontitis. Further clinical studies with diverse initial diagnoses are necessary, although cryotherapy is likely to yield similar effects in pain reduction. Moreover, it can be supplemented with other methods to achieve this objective.
As of now, there is no specific clinical protocol established regarding the ideal temperature of the irrigant, the most suitable one, and the application duration. Cryotherapy proves to be an easily applicable method with few contraindications, non-toxic, and requiring minimal economic investment from professionals. Additional clinical studies should be conducted to investigate the effect of cryotherapy on tooth fracture resistance, which poses a limitation in its application due to the less conclusive findings of in vitro studies.
REFERENCES
1. Lasala A. Introducción. En: Endodoncia, 4ª ed. Barcelona: Ediciones Cientificas y Tecnicas SA Elsevier, 1992, p.xv.- xvi. [ Links ]
2. Maisto OA, Endodoncia. En: Endodoncia, 4ª ed. Buenos Aires: Editorial Mundi, 1984. p.1-8. [ Links ]
3. Pita L, Matos D, Tabera M, Martínez A, Morejón D. Estados inflamatorios pulpares más frecuentes en servicios de urgencia. Rev Inf Cient. 2017; 96(4): 636-645. [ Links ]
4. Fayyad D, Abdelsalam N Hashem N. Cryotherapy: A New Paradigm of Treatment in Endodontics. J Endod 2020; 46(7): 936-942. [ Links ]
5. Vera J, Ochoa J, Vazquez M, Romero M, Arias A, Sleiman P. Effect of Intracanal Cryotherapy on Reducing Root Surface Temperature. J Endod 2015; 41(11): 1884-1887. [ Links ]
6. Gutiérrez H, Lavado I, Méndez S. Revisión sistemática sobre el efecto analgésico de la crioterapia en el manejo del dolor de origen músculo esquelético. Rev Soc Esp Dolor. 2010; 17(5): 242-252. [ Links ]
7. Vidal J. Versión actualizada de la definición de dolor de la IASP: un paso adelante o un paso atrás. Rev Soc Esp Dolor 2020; 27(4): 232-233. [ Links ]
8. Gupta A, Aggarwal V, Gurawa A, Mehta N, Abraham D, Singh A, Jala S, Chauhan N. Effect of intracanal cryotherapy on postendodontic pain: a systematic review and meta-analysis of randomized controlled trials. J Dent Anesth Pain Med 2021; 21(1): 15-27. [ Links ]
9. Lobo Cortés L, Rebolledo Cobos M, Mejía Fernández P. A propósito de la crioanestesia dental. Revista Cubana de Estomatología 2020 57(4): e3074. [ Links ]
10. Gundogdu E, Arslan H. Effects of Various Cryotherapy Applications on Postoperative Pain in Molar Teeth with Symptomatic Apical Periodontitis: A Preliminary Randomized Prospective Clinical Trial. J Endod 2018; 44(3): 349-354. [ Links ]
11. Rivera-Lara L, Zhang J, Muehlschlegel S. Therapeutic hypothermia for acute neurological injuries. Neurotherapeutics. 2012 Jan; 9(1): 73-86. [ Links ]
12. Keskin C, Ozdemir O, Uzun I, Bugra Guler B. Effect of intracanal cryotherapy on pain after single-visit root canal treatment. Aust Endod J 2017; 43: 85-90. [ Links ]
13. Nadler S, Weingand K, Kruse R. The Physiologic Basis and Clinical Applications of Cryotherapy and Thermotherapy for the Pain Practitioner. Pain Physician 2004; 7(3) 395-399. [ Links ]
14. Farah C, Savage N. Cryotherapy for treatment of oral lesions. Aust Dent J 2006; 51: (1): 2-5. [ Links ]
15. Karthikeyan S, Vinayachandran D. "Cryotherapy"- A Panacea for Post-Operative Pain Following Endodontic Treatment. Acta Scientific Dental Sciences 2017; 1(1): 01-03. [ Links ]
16. Vera J, Ochoa J, Romero M, Vazquez M, Ramos C, Rosas R, Cruz A, Sleiman P, Arías A. Intracanal Cryotherapy Reduces Postoperative Pain in Teeth with Symptomatic Apical Periodontitis: A Randomized Multicenter Clinical Trial. J Endod 2018; 44(1): 4-8. [ Links ]
17. Rodríguez O, García L, Bosch A, Inclán A. Fisiopatología del dolor bucodental: una visión actualizada del tema. MEDISAN 2013; 17(9): 5079- 5085. [ Links ]
18. Braga L, Marcella, Reis M, de Castro R, Baraúna M, Cople L , Melo da Silva J. Effect of intracanal cryotherapy application on postoperative endodontic pain: a systematic review and metaanalysis. Clin Oral Invest 2021; 25: 23-35. [ Links ]
19. Vandana G, Digesh B, Reema A, Rachana G, Jaykumar G: Cryotherapy: An Emerging Trend in the Field of Endodontics.Int. J. Drug Res. Dental Sci., 2020; 2(3): 70-76. [ Links ]
20. Nandakumar M, Nasim I. Effect of intracanal cryotreated sodium hypochlorite on postoperative pain after root canal treatment. A randomized controlled clinical trial. J Conserv Dent 2020; 23: 131-6. [ Links ]
21. Di Spirito F, Scelza G, Fornara R, Giordano F, Rosa D, Amato A. Post-Operative Endodontic Pain Management: An Overview of Systematic Reviews on Post-Operatively Administered Oral Medications and Integrated Evidence-Based Clinical Recommendations. Healthcare (Basel). 2022; 10(5):760. Publicado 2022 Apr 19. doi:10.3390/healthcare10050760. [ Links ]
22. Paredes Vieyra J, Gradilla Martínez I, Mondaca JM, Jiménez Enriquez Fco. J, Manriquez Quintana M I. Sistema Endovac en endodoncia por medio de presión apical negativa. Revista ADM 2009; 65 (4): 30-34. [ Links ]
23. Emad A, AbdElsalam N, Fayyad D. Influence of Intracanal Cryotherapy on Pro- And Anttinflamatory Mediators Expression Using Different Irrigation Protocols A Randomized Clinical Trial. Official Dental Journal of Suez Canal University 2021; 2(2): 165-174. [ Links ]
24. Leguisamo J, Vidal S, Espinosa X. Crioterapia como una alternativa no farmacológica para el manejo del dolor endodóntico postoperatorio: Una revisión integrativa de la literatura. Research Society and Development 2021; 10(9) 1-9. [ Links ]
26. Bazaid DS, Kenawi LMM. The effect of intracanal cryotherapy in reducing postoperative pain in patients with irreversible pulpitis: a randomized control trial. Int J Health Sci Res. 2018; 8(2): 83-88. [ Links ]
29. Alharthi AA, Aljoudi MH, Almaliki MN, Almalki MA, Sunbul MA. Effect of intra-canal cryotherapy on post-endodontic pain in single-visit RCT: A randomized controlled trial. Saudi Dent J. 2019 Jul;31(3):330-335. [ Links ]
30. Vieyra J, Enriquez F, Acosta F, Guardado J. Reduction of Postendodontic Pain after One visit Root Canal Treatment Using Three Irrigating Regimens with Different Temperature. Niger J Clin Practice 2019; 22(1): 34-40. [ Links ]
31. Keskin C, Sariyilmaz E, Keles A, et al. Effect of intracanal cryotherapy on the fracture resistance of endodontically treated teeth. Acta Odontol Scand 2019; 77(2): 164-167. [ Links ]
32. Yadav S, Goud V, Paturu P, Ateeq Z, Shilpa A, Yeligati P. Evaluation of Postoperative Pain After Various Cryotherapy Aapplications in Teeth With Chronic Irreversible Pulpitis an in Vivo Study. Int J Med Sci Diag Res 2020; 4(2): 9-11. [ Links ]
34. Jaiswal S, Vagarali H, Pujar M, Kapshe N. Effect of cold saline irrigation on postoperative pain - A randomized control trial. Indian J Conservative Endod 2020; 5(2): 58-62. [ Links ]
36. Abbas Rizvi I, Randhawa S. Eficacia de la irrigación con solución salina fría en el dolor posoperatorio después del tratamiento del conducto radicular: un estudio clínico. J Mar Dent Sci 2021; 4(3): 1-7. [ Links ]
37. Jain A, Chauhan S, Bahuguna R, Agarwal A, Sharma R, Khan F. Effect of Cryotherapy on Postoperative Pain: Randomized Controlled Trial. Indian J Dent Sci 2021; 13(4): 236-240. [ Links ]
38. Jain S, Chokshi S, Sanghvi Z , Trivedi P, Mehta P, Parikh A. Effect of intracanal cryotherapy on fracture resistance of teeth that have undergone endodontic treatment-An in vitro study. J Adv Med Dental Sci Res 2021; 9(1): 31-34. [ Links ]
39. Prithviraj, Vishnuja N, Kumar S, Avinash S, Ganga A, Chincholi R. Effectiveness of Cold Saline Irrigation on Postoperative Pain - An In - Vivo Study. Annals R.S.C.B. 2021; 25(6): 5253-5258. [ Links ]
40. Akpinar KE, Kaya F. Efecto de diferentes prácticas clínicas sobre el dolor posoperatorio en molares mandibular permanentes con periodontitis apical sintomática: un ensayo clínico controlado aleatorizado. Níger J Clin Pract 2021; 24: 8-16. [ Links ]
41. Emad A, Abdelsalam N, Fayyad D. Influence of intracanal cryotherapy on postendodontic pain and interleukin 6 expression using different irrigation protocols: A randomized clinical trial. Saudi Endod J 2021; 11(2): 246-251. [ Links ]
42. Western J, Zahir A, Binti Haja Mohainuteen A, Ping B, Hui C, Ru C, et al. Intracanal cryotherapy with two different temperature ranges in reducing postendodontic pain: A double-blind randomized clinical trial. Saudi Endod J 2022; 12: 82-9. [ Links ]
43. Keskin C, Aksoy A, Kalyoncuoglu E, Keles A, Arkan Ilik A, Kömeç O, Yüzgüleç E| Akgün H ,Alak S, Tokur O. Effect of intracanal cryotherapy on the inflammatory cytokine, proteolytic enzyme levels and post-operative pain in teeth with asymptomatic apical periodontitis: A randomized clinical trial. Int Endod J. 2023; 00:1-11. [ Links ]
44. Allan R, Malone J, Alexander J, Vorajee S, Ihsan M, Gregson W, Kwiecien S, Mawhinney C. Cold for centuries: a brief history of cryotherapies to improve health, injury and post-exercise recovery. Eur J Appl Phisiol 2022 122: 1153-1162. [ Links ]
45. Talal A, Talaat A, Mahmoud A, Ahmad A. Effect of Intracanal Cryotherapy and Negative Irrigation Technique on Postendodontic Pain. J Contemp Dental Pract 2016; 17(12): 990-996. [ Links ]
46. Sadaf, D., Ahmad, M. Z., & Onakpoya, I. Effectiveness of intracanal cryotherapy in root canal therapy: A systematic review and meta-analysis of randomized clinical trials. J Endod 2020; 46(12): 1811-1823. [ Links ]
47. Garcias F, Silva L, Lívia Alves An, Santos Antunes, L. Effect of intracanal cryotherapy on postoperative pain after endodontic treatment: systematic review with meta-analysis. Restor Dent Endod. 2022; 47(3): 1-15. [ Links ]
48. Pauletto G, De Carlo M. Efeito da crioterapia intracanal no controle da dor pós-operatória após terapia endodôntica: uma revisão de literatura. Revista da Faculdade de Odontologia de Porto Alegre 2021; 62 (2): 122-132. [ Links ]
Conflict of Interest Statement: The authors declare no conflicts of interest regarding the publication of this article.
Authorship Contribution Note: a) Study conception and design b) Data acquisition c) Data analysis d) Results discussion e) Manuscript drafting f) Approval of the final version of the manuscript Carlos Perez contributed to: a, b, c, d, e, f Enrique Rotemberg contributed to: b, c, d, e, f
Received: November 03, 2023; Accepted: March 15, 2024










 text in
text in