Servicios Personalizados
Revista
Articulo
Links relacionados
Compartir
Ciencias Psicológicas
versión impresa ISSN 1688-4094versión On-line ISSN 1688-4221
Cienc. Psicol. vol.18 no.2 Montevideo dic. 2024 Epub 01-Dic-2024
https://doi.org/10.22235/cp.v18i2.3598
Original Articles
Perceived parental bonding and variables associated with maternal-fetal attachment in high-risk pregnancy
1 Universidade Federal de Santa Catarina, Brasil, henriquereis@ufba.br
2 Universidade Federal da Bahia, Brasil
3 Universidade Federal da Bahia, Brasil
4 Universidade Federal da Bahia, Brasil
This study investigated the effects of perceived parental bonding, sociodemographic and gestational variables on the intensity of maternal-fetal attachment (MFA) in the context of high-risk pregnancies. This is a quantitative, cross-sectional study involving 119 participants. A sociodemographic questionnaire, the Maternal-Fetal Attachment Scale-Brief Version, and the Parental Bonding Instrument were administered. The results of the multiple linear regression analysis were statistically significant (p < .05). The final model explained 28.7 % of the variance in MFA and included the variables of paternal overprotection, paternal care, maternal age, gestational age, and the support from the baby's father. We emphasize that MFA intensity is multidetermined, involving aspects of life history, social, and situational factors. The woman’s perception of paternal bonding during her childhood and adolescence, as well as the support from the baby's father during the gestational period, are highlighted as influential factors for maternal-fetal attachment, indicating the importance of paternal involvement throughout the life cycle. Implications for professional practice, as well as limitations and recommendations for future studies are discussed.
Keywords: maternal-fetal relations; high-risk pregnancy; family relations; pregnancy
Este estudo investigou os efeitos da percepção do vínculo parental, variáveis sociodemográficas e gestacionais na intensidade do apego materno-fetal (AMF) no contexto de gestação de alto risco. Trata-se de um estudo quantitativo e transversal com 119 participantes. Foi aplicado um questionário sociodemográfico, a Escala de Apego Materno-Fetal - Versão Breve e o Parental Bonding Instrument. Os resultados da análise de regressão linear múltipla foram estatisticamente significativos (p < 0,05). O modelo final explicou 28,7 % da variância do AMF e foi composto pelas variáveis de superproteção paterna, cuidado paterno, idade da mulher, idade gestacional e suporte do pai do bebê. Reitera-se que a intensidade do AMF é multideterminada, envolvendo aspectos da história de vida, sociais e situacionais. A percepção da mulher acerca do vínculo paterno durante sua infância e adolescência e o apoio do pai do bebê no período gestacional destacam-se como fatores influentes para a vinculação materno-fetal, indicando a importância do envolvimento paterno ao longo do ciclo vital. São pontuadas implicações para a prática profissional, bem como limitações e recomendações de estudos futuros.
Palavras-chave: relações materno-fetais; gravidez de alto risco; relações familiares; gestação
Este estudio investigó los efectos de la percepción del vínculo parental, las variables sociodemográficas y gestacionales en la intensidad del apego materno-fetal (AMF) en el contexto de embarazos de alto riesgo. Se trata de un estudio cuantitativo y transversal con 119 participantes. Se aplicó un cuestionario sociodemográfico, la Escala de Apego Materno-Fetal-Versión Breve y el Instrumento de Vínculo Parental. Los resultados del análisis de regresión lineal múltiple fueron estadísticamente significativos (p < .05). El modelo final explicó el 28.7 % de la varianza del AMF y estuvo compuesto por las variables de sobreprotección paterna, cuidado paterno, edad de la mujer, edad gestacional y apoyo del padre del bebé. Se reitera que la intensidad del AMF es multideterminada, lo que involucra aspectos de la historia de vida, sociales y situacionales. La percepción de la mujer sobre el vínculo paternal durante su infancia y adolescencia, así como el apoyo del padre del bebé durante el período gestacional, destacan como factores influyentes en el apego materno-fetal, lo que indica la importancia de la participación paterna a lo largo del ciclo vital. Se puntualizan implicaciones para la práctica profesional, así como limitaciones y recomendaciones para estudios futuros.
Palabras clave: relación materno-fetal; embarazo de alto riesgo; relaciones familiares; embarazo
Pregnancy is a natural process of human development that involves physical, hormonal, emotional, and social changes for the pregnant woman, which necessitate a restructuring of identity and an adaptation to new parental roles (Papalia & Martorell, 2022). Beyond attitudes and behaviors evolutionarily selected to ensure the survival of offspring and, ultimately, the species, the mother-baby relationship encompasses particular aspects of her internal world and evokes pre-pregnancy experiences, such as the care received in childhood and parental models (Balle, 2017; Trombetta et al., 2021). This relationship begins during intrauterine life, as throughout the gestational period, the baby is impacted by the external world and the mother's experiences (Lucena et al., 2019; Rosa et al., 2021).
Although most pregnancies occur without major complications, about 20 % of women in Brazil experience comorbidities and risks during this period (Alves et al., 2021). High-risk pregnancy occurs when the gestational process poses risks to the health of the mother and/or the fetus, and certain factors can increase the likelihood of its occurrence (Gadelha et al., 2020). Risk factors are related to individual characteristics, unfavorable sociodemographic conditions, previous reproductive history, obstetric diseases in the current pregnancy, and clinical complications (Rodrigues et al., 2017). These aspects can trigger stress and negatively affect the mental health of the pregnant woman, potentially impacting the bonding process with the baby and consequently leading to impairments in the child's development, as well as difficulties in the process of adapting to motherhood (Topan et al., 2022).
Considering the importance of mother-infant bonding for healthy development, Cranley (1981) defined the attachment/bond established by the mother toward the fetus as "maternal-fetal attachment" (MFA). It is characterized by the intensity of the woman's attitudes during pregnancy related to the establishment of a bond and closeness with the fetus, involving cognitive and affective aspects, as well as her attributions regarding the fetus's physical and emotional characteristics (Suryaningsih et al., 2020; Trombetta et al., 2021). The development of MFA is an important component in the process of forming and adapting to motherhood, potentially influencing the pregnancy experience and the quality of the mother-child relationship after birth (Ponti et al., 2021; Sacchi et al., 2021).
Review studies indicate that MFA functions as a predictor of healthy emotional, behavioral, cognitive, and social development in early childhood, and that mothers who developed stronger MFA tend to be less self-critical, more engaged in healthy behaviors during pregnancy, and less vulnerable to negative psychological symptoms (Rollè et al., 2020; Trombetta et al., 2021). MFA is also associated with a greater perception of competence regarding parental care in the postpartum period, increased maternal sensitivity in identifying the newborn's needs, and better adaptation to motherhood (Çelik & Güneri, 2020; Göbel, 2019).
The development of maternal-fetal attachment is multidimensional, influenced by socioeconomic variables, the quality of the marital relationship, the pregnant woman's education, gestational age, and social support (Cheraghi & Jamshidimanesh, 2022; Sacchi et al., 2021; Topan et al., 2022). Review studies highlight social support (from family and partner) as an important contextual variable in determining the intensity of MFA, with greater perceived support being associated with stronger maternal-fetal bonding and a smoother transition to motherhood (Cerqueira et al., 2023; Yarcheski et al., 2009). However, another determining factor is the pregnant woman's own attachment history with her caregivers. This is a foundational aspect of personality, contributing to the development of internal functioning modes (mental representations or beliefs that guide an individual’s perception and behavior) and to her attitudes toward parental care (Gioia et al., 2023; Rosa et al., 2021).
According to Attachment Theory, the quality and dynamics of the relationship established with primary caregivers, especially during childhood and adolescence, contribute to the formation of internal working models. These are mental representations the child creates about the environment, themselves, and relationships (Karantzas et al., 2023). Such models evolve with the child's development and begin to function as guides for interpreting events and relationships throughout life, thereby integrating into their personality (Fraley & Roisman, 2019; Selcuk et al., 2024). As they involve both affective and cognitive aspects, they tend to have a strong impact on interpersonal relationships, attachment processes, self-construction, and the exercise of parenthood (Richter et al., 2022; Sacchi et al., 2021). During pregnancy, it is common for women to revisit memories and perceptions of their attachment to parental figures. This process may influence how they perceive themselves as mothers and their closeness to the child, with the possibility of reworking and assigning new meanings to these memories during pregnancy (Balle, 2017; Handelzalts et al., 2018; Hinesley et al., 2020).
Although attachment theory proposes that the quality and intensity of primary attachment influence other bonds throughout life, there are still few empirical studies that have sought to evaluate the relationships between primary attachment and MFA, especially in the context of high-risk pregnancies (Cerqueira et al., 2023; Handelzalts et al., 2018; Sacchi et al., 2021). Cerqueira et al. (2023) conducted a review study aimed at investigating the scientific literature on MFA in high-risk pregnancies and emphasized the need for research that also considers the pregnant woman's attachment history as an influential factor, highlighting the absence of studies with this objective and population, particularly in the Brazilian context. Furthermore, in a literature review over the last 13 years conducted by the authors of the present study, only ten studies were found relating primary attachment to maternal-fetal attachment. Of these, only two (Balle, 2017; Handelzalts et al., 2018) included high-risk pregnant women in their sample. However, no group comparisons or distinct analyses considering gestational risk were conducted, making it impossible to assess whether the relationships between variables and outcomes behave similarly in both conditions.
Two studies found were conducted in Brazil (Balle, 2017; Rosa et al., 2021). In a study with 839 pregnant women without gestational risk, Rosa et al. (2021) investigated the explanatory power of sociodemographic, gestational, and primary attachment variables (using the Parental Bonding Instrument, PBI) in the intensity of MFA through regression analyses. Pregnant women in their first trimester, who were not living with a partner and who did not feel supported by the baby’s father during pregnancy showed lower MFA scores. However, after controlling for these variables, paternal overprotection was a positive predictor of MFA, while the other primary attachment dimensions (Maternal and Paternal Care and Maternal Overprotection) did not show statistically significant relationships. It is worth noting that all study participants exhibited high levels of MFA, regardless of their perception of parental attachment, indicating that during pregnancy, a woman may bond with her baby even without positive childhood memories.
Still in the Brazilian context, Balle (2017) conducted a study with 364 pregnant women, of whom 14 % were considered high risk, to identify the relationships between MFA and sociodemographic variables, prenatal care, and the care factor of the PBI. In a correlation analysis, the author found a positive but weak association only with maternal care. Through regression analysis, this same factor explained 5.1% of the variance in MFA. Although it did not indicate a significant association between high-risk pregnancies and maternal-fetal attachment, this variable was positively related to gestational age and negatively related to the mother's age.
In a longitudinal study with 1,301 pregnant women without gestational risk, Fukui et al. (2021) investigated the relationships between primary attachment (PBI), maternal-fetal attachment, and indicators of mental health. Through path analysis, they indicated that the perception of low maternal and paternal care negatively affected the bond with the baby, and this effect persisted after childbirth. However, the authors did not discuss the possible effects of sociodemographic (e.g., age) or gestational variables (e.g., primiparity and gestational age) on these relationships. In contrast, Gioia et al. (2023), using a sample of 1,177 pregnant women and regression analyses, indicated that gestational age, primiparity, and perceptions of paternal and maternal care (assessed through the PBI) were statistically significant predictors of maternal-fetal attachment. It is worth noting that this relationship was not mediated by indicators of mental health (e.g., anxiety and depression), suggesting direct effects. Van Bussel et al. (2010) reported similar results based on positive but weak correlations between paternal care and MFA in a sample of 403 pregnant women. No significant relationships were found with other sociodemographic or gestational variables.
Sacchi et al. (2021) investigated the association between MFA, mental health, marital relationship, and maternal primary attachment using a sample of 113 low-risk pregnant women. Through correlation and regression analyses, maternal care was positively related to MFA, as was the quality of the marital relationship. The authors indicated that the pregnant woman's past and current relationships serve as models for her maternal representations regarding her relationship with the baby, impacting the attachment. In agreement, Handelzalts et al. (2018) also found a positive correlation between MFA and maternal care in a study with 341 pregnant women, 17.4 % of whom were in high-risk pregnancies. However, when regression analysis was conducted, women with high scores in the Care and Denial of Autonomy factors of maternal attachment also exhibited stronger MFA. Other factors associated with greater intensity of MFA included younger age, lower education, and fewer previous births. In the study, no significant associations were found between high-risk conditions and maternal-fetal attachment.
In a study with 101 pregnant women, Hinesley et al. (2020) investigated the impact of exposure to adverse childhood experiences on maternal variables such as primary attachment, MFA, and mental health through path analysis. Regarding MFA, positive direct relationships were identified only with paternal care and the age of the pregnant woman. No direct associations were found between adverse experiences (e.g., neglect and coercion) in childhood and MFA. However, the low perception of paternal care explained part of the negative indirect effect of these adverse experiences on MFA. Concerning primary attachment, high exposure to adverse events in childhood was negatively associated with the perception of paternal and maternal care and was a significant predictor of perceiving both parents as intrusive and controlling.
The study by Teixeira et al. (2016) analyzed the relationship between MFA, gestational age, and memories of parenting practices (using the Memories of Parenting Practices Scale, EMBU) in 179 pregnant women. Through correlation analyses, it was found that perceived rejection by both the father and the mother is associated with lower MFA, specifically with a decreased identification of the pregnant woman as a future mother. The authors also reported a positive association between gestational age and MFA. Finally, in examining the relationship between maternal factors and prenatal attachment in a sample of 32 pregnant women, Reed (2014) identifies the combination of lower care and greater overprotection from the primary caregiver, whether the mother or the father, as a risk factor for lower maternal-fetal attachment, particularly in pregnant women with low educational attainment. Furthermore, using analysis of variance (ANOVA), pregnant women who reported high social support, lack of religious affiliation, low anxiety, and low dependence in current adult relationships demonstrated higher MFA.
It is evident that there is a diversity of results found in the studies, indicating the need for future investigations. It is worth noting that research utilizing high-risk pregnant women as a sample is even scarcer, and such studies have not sought to investigate the perception of parental attachment as a possible predictor, considering only gestational, marital, sociodemographic, and mental health information (Cerqueira et al., 2023; Cheraghi & Jamshidimanesh, 2022; Soares et al., 2022; Topan et al., 2022). Thus, this study aimed to investigate the effects of the perception of primary attachment, sociodemographic and gestational variables on the intensity of MFA in a high-risk pregancy context.
Method
This is a quantitative, cross-sectional study with non-probabilistic convenience sampling. Data collection took place between February and May 2023 at a maternal and child hospital located in the city of Vitória da Conquista, Bahia. The facility provides medium- and high-complexity services to pregnant women from the southwestern region of the state, as well as psychological care by professionals in the field.
Participants
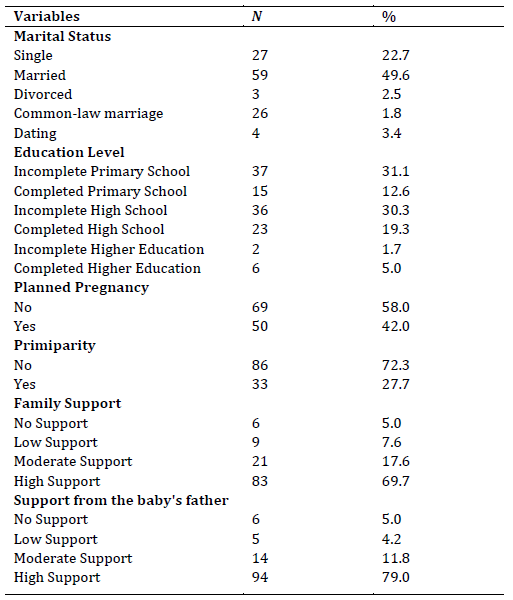
A total of 119 pregnant women aged between 18 and 45 years (M= 30.45; SD= 6.58) and gestational ages between 27 and 40 weeks (M= 32.53; SD= 4.03), all of whom were undergoing high-risk prenatal care, participated in the study. The inclusion criteria required participants to be over 18 years old and at least in their 27th week of pregnancy, as maternal-fetal bonding becomes more evident from this period onward (Lima et al., 2022; Rosa et al., 2021). To be classified as "high-risk", the pregnant woman had to be diagnosed by a medical professional indicating such a condition. There were no restrictions or categorizations regarding the different conditions (e.g., hypertension, gestational diabetes) that could lead to a high-risk pregnancy diagnosis. Pregnant women with cognitive developmental delays, moderate/severe hearing loss, or muteness (aphonia) were excluded, as the instruments used do not have adaptations for the specific needs of these populations. Table 1 presents the participants' characteristics in terms of marital status, education, family support, support from the baby's father, pregnancy planning, and primiparity.
Instruments
Sociodemographic Questionnaire. Developed by the authors, this questionnaire included questions regarding age, gestational period, among others, aiming to understand the conditions of pregnancy and characterize the sample. Two additional questions related to social support were included, where participants were asked to rate, on a Likert scale from 0 (No Support) to 3 (High Support), their perception of the support received from their family (“How do you perceive the level of support you are receiving from your family during this pregnancy?”) and from the baby’s father (“How do you perceive the level of support you are receiving from the baby’s father during the current pregnancy?”).
Parental Bonding Instrument (PBI; Teodoro et al., 2010). The scale is designed to assess the quality of the bond between parents and their children during childhood and adolescence, based on Attachment Theory. This theoretical model posits that early interactions with caregivers have a long-term impact on psychological development. In Brazil, Teodoro et al. (2010) conducted a validation study, confirming the factorial validity and internal consistency of the PBI. The instrument consists of two main factors: Care (12 items) and Overprotection/Control (13 items). Responses are given on a Likert scale (ranging from 0 to 3), and the scores are separated into maternal and paternal versions, with a maximum score of 36 points for the Care scale and 39 points for the Overprotection/Control scale. Regarding internal consistency, Cronbach's alphas were 0.91 for Care and 0.87 for Overprotection/Control in the maternal relationship, and 0.91 and 0.85 in the paternal relationship, respectively.
Maternal-Fetal Attachment Scale - Short Version (MFAS; Escala de Apego Materno-Fetal - Versão Breve; Lima et al., 2022). Developed by Cranley (1981), the scale assesses the bond between the pregnant woman and the fetus. A brief version of this scale was adapted and validated for Brazil by Lima et al. (2022) in a study involving 937 pregnant women in the second and third trimesters of pregnancy. The values obtained showed a Cronbach's alpha of .878 and a composite reliability > .70, indicating appropriate psychometric properties. The scale consists of 15 items rated on a Likert scale ranging from 1 (Strongly disagree) to 5 (Strongly agree) and is divided into three factors: “Experiencing Expectations,” “Interactions with the Fetus,” and “Imagination and Care for the Baby.” The total score ranges from 15 to 75, with higher values indicating a greater intensity of attachment. In the present study, following recommendations from previous research (Gioia et al., 2023; Lima et al., 2022; Rosa et al., 2021; Sacchi et al., 2021), the total score was used instead of the three factors of the scale.
Procedures
Data collection
Pregnant women awaiting high-risk prenatal care were invited to participate in the study by interns and extension students associated with the Núcleo de Especializado de Estudos em Desenvolvimento Humano (NEEDH) of the Universidade Federal da Bahia - Instituto Multidisciplinar em Saúde (UFBA-IMS), who had been previously trained by psychologists from the hospital. All women receiving care at the hospital had a diagnosis of high-risk pregnancy. There was no pre-defined criterion regarding which women in the waiting room would be approached. After the initial contact, if the pregnant women met the inclusion criteria and agreed to participate in the study, they were informed that their contribution was voluntary and that declining to complete the instruments would not result in any disadvantage to the hospital care they received.
The Written Informed Consent Form (WICF) was read before the administration of the instruments, and only those who agreed to the document participated in the study. During the reading of the WICF, the participants were informed about the risk of emotional discomfort due to the investigated theme, and those who exhibited such reactions were supported by the researchers and referred to the hospital's psychology service for follow-up with the service's professional staff. After providing consent, the participants were individually interviewed by the researchers in the waiting room for approximately 30 minutes.
Data analysis
The collected data were analyzed using the Statistical Package for the Social Sciences (SPSS) version 25. Descriptive statistics were employed to calculate frequency measures, means, and standard deviations. Subsequently, a correlation analysis was conducted between the predictor variables, utilizing Cohen's (1992) criteria for interpreting the correlation coefficient r. Thus, weak correlations (r ≤ .29), moderate correlations (.30 ≤ r ≤ .49) and strong correlations (r ≥ .50) were considered.
Following this, to investigate the determinants of maternal-fetal attachment (outcome variable), a multiple linear regression analysis was conducted using the backward entry method. In this method, all predictor variables are entered simultaneously into the initial regression model. The program evaluates the statistical significance of each variable through the p-value, and those that are not significant are automatically removed to create a more parsimonious model. This process is repeated until all remaining variables contribute statistically significantly to the explanation of the outcome variable.
For the selection of predictor/explanatory variables included in the regression model, previous studies were used as a basis (Cheraghi & Jamshidimanesh, 2022; Gioia et al., 2023; Handelzalts et al., 2018; Rosa et al., 2021; Sacchi et al., 2021; Soares et al., 2022; Topan et al., 2022). The following variables were included: sociodemographic variables (education and age), gestational variables (gestational age, primiparity, pregnancy planning, family support, and support from the baby's father), and perception of parental bonding (Maternal Overprotection, Maternal Care, Paternal Overprotection, and Paternal Care). Relationships were considered significant at p ≤ .05. The following assumptions of multiple linear regression were verified: absence of multicollinearity among the independent variables (variance inflation factor, VIF, close to 1), normality of the distribution of residuals (Lilliefors Test with p> .05) and independence among the residuals (Durbin-Watson coefficient between 1.5 and 2.5) (Mourão et al., 2021).
Ethical procedures
The study received favorable approval from the Research Ethics Committee (CEP) of the Universidade Federal da Bahia (UFBA) through registration number 5.732.443 (CAAE: 62798622.3.0000.5556). All information from the WICF was read to the participants before the application of the questionnaires, and only those pregnant women who agreed and voluntarily signed the WICF were included in the research.
Results
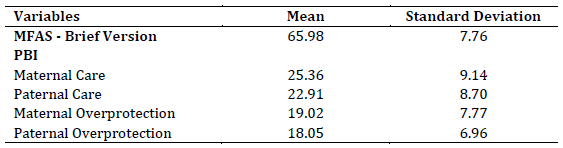
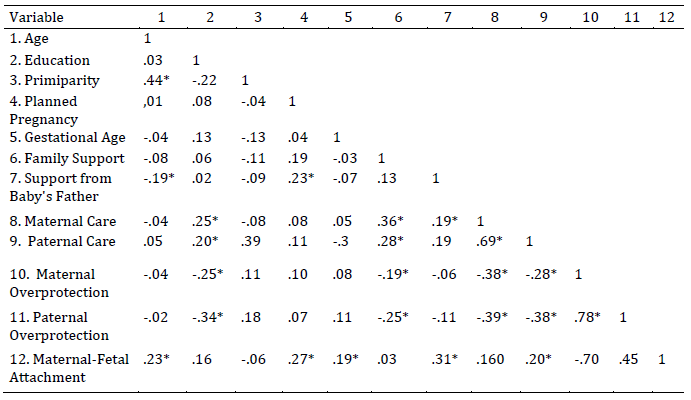
The first results analyzed were the descriptive statistics of maternal-fetal attachment (MFAS-Brief Version) and the perception of parental bonding (PBI). The values are presented in Table 2. Subsequently, correlations were performed among sociodemographic variables, gestational variables, the perception of parental bond, and maternal-fetal attachment. The results are presented in Table 3.
Table 3: Correlations between sociodemographic variables, gestational variables, erceived parental bonding, and maternal-fetal attachment
*p < .05
The analyses indicated weak and positive correlations of maternal-fetal attachment (MFA) with age, planned pregnancy, gestational age, and paternal care, as well as a moderate and positive correlation with support from the baby's father. Strong correlations were observed between maternal overprotection and paternal overprotection, as well as between maternal care and paternal care. Family support showed weak and negative correlations with both maternal and paternal overprotection, and a strong positive correlation with maternal care.
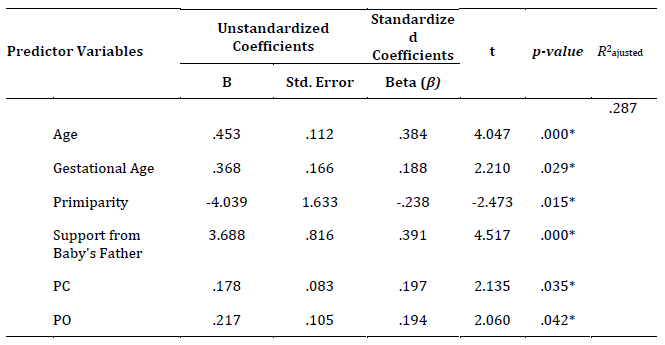
Subsequently, a multiple linear regression analysis was conducted with maternal-fetal attachment (MFA) as the outcome variable. To perform the analysis, it was necessary to verify the assumptions of regression. The result of the Kolmogorov-Smirnov test (p> .05) indicated the normality of the residuals, the Durbin-Watson coefficient (D) was equal to 1.993, and the variance inflation factor (VIF) values ranged from 1.04 to 1.33, indicating that the data meet the necessary criteria for the analysis to be conducted. Table 4 presents the process of variable insertion and removal using the backward method.
Table 4: Variables inserted and removed in the regression models
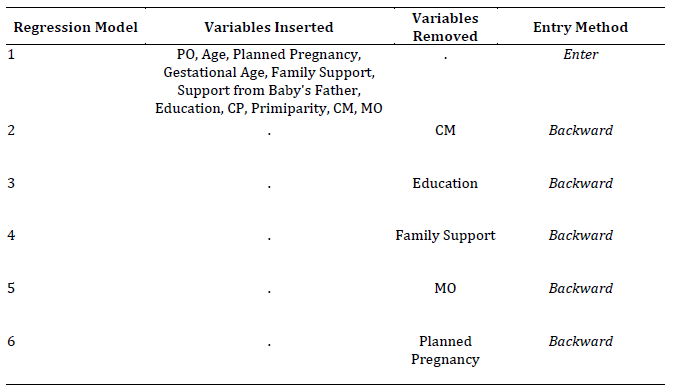
Notes: CP: Paternal Care; CM: Maternal Care; PO: Paternal Overprotection; MO: Maternal Overprotection.
The final model (6) of the multiple linear regression analysis (backward method) with maternal-fetal attachment (MFA) as the outcome variable showed a statistically significant result (F (6, 97) = 7.893; p < .001; R 2 ajusted = .287), explaining 28.7 % of the variance in MFA. The variables included in this model, in descending order of individual contribution (standardized coefficient β), were: support from the baby's father, age, primiparity, paternal care, paternal overprotection, and gestational age. The regression coefficients that comprised the final model are shown in Table 5.
Discussion
The present study aimed to evaluate the effects of the perception of primary bonding, sociodemographic and gestational variables on the intensity of maternal-fetal attachment in high-risk pregnant women. The results indicated that the perception of overprotection and paternal care during childhood and adolescence were significant predictors of a higher intensity of maternal-fetal attachment (MFA). These findings reinforce the role of paternal involvement during childhood and adolescence, which may have repercussions in the transition to parenthood (Diniz et al., 2021). Empirical studies support positive relationships between greater paternal involvement/engagement and child development, such as lower rates of behavioral and psychological problems, better cognitive functioning, and positive self-concept (Diniz et al., 2021; Henry et al., 2020; Rollè et al., 2020). Indeed, the results of this study align with other works (Fukui et al., 2021; Gioia et al., 2023; Handelzalts et al., 2018; Hinesley et al., 2020; Rosa et al., 2021; van Bussel et al., 2010), although these studies did not explore the reasons or mechanisms by which memories of maternal and paternal bonds differentially affect MFA intensity. These results were also found in studies with low-risk pregnant women, indicating that gestational risk may not be a variable that affects the relationship between primary attachment and MFA (Cerqueira et al., 2023).
The pregnant woman's perception of the care and overprotection received from her father may be associated with a greater presence of this figure in her life, contributing to the formation of a secure attachment characterized by feelings of safety, protection, and support. These memories can make the pregnant woman feel more prepared to offer the same care to her child, reflecting in the intensity of maternal-fetal attachment (MFA; Rosa et al., 2021). It is important to note that the roles of the father and mother may be perceived and remembered differently depending on the culture and life history of the pregnant woman. Maternal care and greater involvement are often naturalized, as mothers are traditionally viewed as the primary caregivers responsible for family well-being (Schmidt et al., 2023). In contrast, the participation of fathers (paternal figures) in caregiving may be perceived as a supportive or complementary role to that of the mother, with lower cultural expectations regarding the exercise of their fatherhood and responsibilities (Cabrera et al., 2018; Diniz et al., 2021; Grossmann et al., 2008). Thus, when the paternal figure assumes a more active role in caregiving and consequently has greater involvement in the life of the child/adolescent, it is possible that there is a deeper emotional and affective impact, leading to a greater appreciation of these memories during pregnancy.
The factors of care and overprotection investigated in the present study were initially described by Parker et al. (1979) in an attempt to more precisely define the construct of parental attachment, proposing that both are composed of two poles (high and low). Care is presented as the primary dimension of attachment and is characterized, at the high level, by emotional warmth, closeness, affection, empathy, and fondness, while at the low end it denotes emotional coldness, rejection, and indifference. Overprotection, in turn, is defined as control, surveillance, excessive contact, and infantilization at its high level, and at its low pole, it signals encouragement of independence and autonomy. Although high overprotection has been pointed out as a significant variable of problematic outcomes in areas of children's behavior, such as social skills, self-esteem, and mental health (Ferreira, 2016; Martins et al., 2014; Richter et al., 2018; Wendt & Appel-Silva, 2020), it may be related to an important parental task: the establishment of rules and limits (Handelzalts et al., 2018). This perception supports the positive influence between this factor and more intense maternal-fetal attachment (MFA), as found in the present study and in the research by Fukui et al. (2021), Rosa et al. (2021), and Handelzalts et al. (2018).
Other explanatory models of parenting practices (Baumrind, 1966; Gomide, 2006; Maccoby & Martin, 1983) indicate that high demand, positive monitoring of behavior, and consistent discipline are assertive components of parenting that influence lower levels of emotional problems, as well as higher rates of prosocial behaviors and self-esteem (Bhide et al., 2019; Martins et al., 2014; Weber, 2017). Thus, despite the potential negative outcomes, paternal overprotection may also be associated with a positive perception of security, contributing to greater concern from the woman for the baby during pregnancy and, consequently, a higher intensity of maternal-fetal attachment (MFA) (Rosa et al., 2021).
In turn, the influence of paternal care on MFA found in the present study aligns with other findings in the literature (Fukui et al., 2021; Gioia et al., 2023; van Bussel et al., 2010). A recent research on the topic, conducted by Gioia et al. (2023), indicated that the care provided by the father was a predictor of the dimensions “assuming a maternal role” and “attributing characteristics to the fetus” of the MFA, also highlighting intergenerational transmission through epigenetics and direct observation as a possible explanation for this phenomenon. Thus, biological mechanisms, such as genetically influenced tendencies (e.g., temperament), may be modulated by the parental care received, either mitigating or enhancing these characteristics. Moreover, the observation of parental care behaviors can serve as a model for the gestational repertoire in her role as a future mother (Provenzi et al., 2020). Such influences may vary in intensity depending on other social factors (e.g., stress, social support), individual factors (e.g., negative affect), and relational dynamics (e.g., family functioning) (Santana & Souza, 2018). Conversely, the perception of parental rejection, which can be compared to the lower pole of care, may undermine the pregnant woman's adaptation to motherhood, influencing a sense of low competence in providing neonatal care and breastfeeding (Teixeira et al., 2016).
It is indicated that the relationship developed by the pregnant woman with the primary caregiver in childhood and adolescence will extend and, consolidating throughout her life cycle, will contribute to the formation and maintenance of future bonds, relationships, and emotional states, tending to repeat or impact the construction and intensity of maternal-fetal attachment (Gioia et al., 2023; Trombetta et al., 2021). It is worth highlighting that the average maternal-fetal attachment in the sample of this study was high (M= 65.98), indicating that even when the perceived parental bond with caregivers is low, it is possible for the pregnant woman to reformulate and attribute new meanings to these experiences. Therefore, the participants were able to bond positively with the fetus and develop greater adaptation to motherhood, especially with the support of the baby’s father, sustaining a non-deterministic perspective of primary attachment (Rosa et al., 2021; Topan et al., 2022).
In a review study with a meta-analysis, Yarcheski et al. (2009) point out that partner support during pregnancy is an important aspect to be considered, having a moderate effect size in predicting the intensity of maternal-fetal attachment (MFA). Additionally, Cuijlits et al. (2019), in research involving 739 pregnant women, also identify partner support as the main protective factor during pregnancy and postpartum, while Sacchi et al. (2021) and McNamara et al. (2019) indicate that the quality of the marital relationship is positively associated with higher MFA. The support of the baby’s father is configured as a specific type of social support that tends to involve more affective and emotional components for the pregnant woman. It can serve as an important protective factor for the adaptation process to motherhood, reducing stress, anxiety, and ambivalent feelings that may be present, thereby promoting maternal self-efficacy (Campbell, 2022). In agreement, the results of our study indicated that the variable “support from the baby’s father” had the most significant impact on the level of MFA (β = .391), reinforcing the importance of greater paternal involvement from pregnancy onwards. It is possible that the perception of this support by the pregnant woman is heightened due to the high-risk pregnancy, which, due to the context of greater uncertainty and concern regarding the child’s health, entails a greater need for paternal support, indicating a bidirectional influence relationship (Rocha et al., 2022; Topan et al., 2022; Yarcheski et al., 2009).
The literature highlights the relevance of the father's role in a healthier pregnancy and postpartum experience, as acceptance of the child and support during pregnancy are associated with significant outcomes in the mother’s sense of self-efficacy and lower levels of maternal psychological distress, which could negatively impact MFA (Papalia & Martorell, 2022). Paternal involvement during prenatal care can yield benefits such as improved family unity (father-mother-child), reduced anxiety and concerns regarding the pregnancy cycle, and greater clarity and acceptance of the changes brought about by pregnancy, as the partner creates a safe and welcoming environment that fosters greater interaction between the mother and the baby (Vieira & Aguiar, 2021). In a review study on MFA in high-risk contexts, Cerqueira et al. (2023) emphasize social support as the main protective factor for positive attachment. Thus, the quality of current relationships and the support received may have a more substantial impact on the maternal-fetal relationship process than memories of parental attachment.
The results also indicated that gestational age positively impacts maternal-fetal attachment (MFA), corroborating other studies that suggest attachment behaviors intensify as pregnancy progresses (Cuijlits et al., 2019; Gioia et al., 2023; Rosa et al., 2021; Yarcheski et al., 2009). This effect is primarily due to increased interaction between the mother-baby dyad starting from fetal movements, greater physical experiences, and the approaching delivery, making the experience of pregnancy more tangible and, consequently, reinforcing the establishment of attachment. The mother’s age was also associated with greater intensity of MFA, aligning with findings from Gioia et al. (2023), McNamara et al. (2019), and Yarcheski et al. (2009), as younger pregnant women may experience more intense ambiguous feelings about pregnancy, facing greater challenges in the adaptation process to motherhood and, consequently, in bonding with the fetus, especially in high-risk pregnancies (Çelik & Güneri, 2020; Cerqueira et al., 2023).
Finally, the factor of primiparity also emerged as an explanatory variable for maternal-fetal attachment (MFA), establishing a negative relationship. Although this finding corroborates the review study conducted by McNamara et al. (2019), which indicates that multiparity is associated with a greater intensity of MFA, Yarcheski et al. (2009) report a moderate to null effect size in the relationship between parity and MFA, which supports the inconclusive nature of the relationship between these variables (Fukui et al., 2021).
Conclusions
This research presents significant contributions to a greater understanding of the factors involved in maternal-fetal attachment (MFA) and the development of psychological practices. This is one of the few studies that sought to evaluate the effects of parental attachment and other variables on MFA, considering high-risk pregnancies a topic still underexplored in the national and international scientific literature with this sample, despite its relevance to public health. First, although most studies focus on the maternal figure and its impact during pregnancy, our results reinforce the importance of the father's role in development. His presence and support can make the attachment process more positive for the mother-baby dyad, contribute to a favorable adaptation to motherhood, and ultimately promote the healthy development of the child. This support can be encouraged by health professionals throughout the entire prenatal, childbirth, and postpartum processes by including partners as a target audience for public policies, such as the Partner Prenatal Program proposed by the Ministry of Health (Ministério da Saúde, 2016). Such process may encompass a welcoming and inclusive stance towards men in health service environments (which are predominantly frequented by women), guidance on relevant topics in the pregnancy and postpartum processes, educational activities to prepare for the role of father, and participation during childbirth, fostering their role as caregivers and attachment figures.
Retrospectively, a woman's bond with her own father during childhood and adolescence also has a significant influence on her parenting practices, with repercussions throughout her life cycle. Our results highlight paternal involvement as an essential protective factor for the healthy development of the child, underscoring the importance of creating interventions that promote the active participation of paternal figures in childcare. Parent guidance groups specifically aimed at men, interventions that strengthen coparental relationships, and psychoeducational strategies that emphasize the relevance of paternal participation in child development are recommended as effective approaches (Gonzalez et al., 2023; Nascimento et al., 2022). Research focusing on the coparental relationship, particularly the phenomenon of maternal gatekeeping, indicates that support and encouragement from the mother are crucial factors for increasing paternal involvement in the child's life (Altenburger, 2022; Campbell, 2022). Such practices can be promoted in prenatal consultations and care, as well as in support groups for expectant mothers, through psychoeducation, reflections on motherhood and fatherhood, and highlighting the importance of social support to reduce overload, stress, and enhance attachment.
Regarding the limitations of this study, we highlight possible memory biases associated with the Parent Bonding Instrument (PBI), as current family support and existing parental relationships may influence the participants' recollections and responses. Furthermore, due to the inability to conduct individual data collection, the context in which the questionnaires were administered (specifically, in the waiting room of a high-risk prenatal care facility) should be considered, as some pregnant women may have felt embarrassed or, due to social desirability, avoided reporting negative experiences with their caregivers and a potentially low maternal-fetal bond. For future studies, it is advisable that data collection occurs in more private settings or is conducted by professionals who already have an established rapport with the participants to minimize these limitations.
We also recommend that new studies include samples composed of both high-risk and healthy pregnant women, with the aim of comparing levels of paternal support in both groups, as well as the involvement of fathers during their partners' pregnancies. Including the fathers of the babies or the partners of the pregnant women as participants, along with investigating their perceptions of their relationship with the pregnant woman and their bond with the baby, may contribute to a deeper understanding of the determinants and, consequently, the encouragement of this support during pregnancy. We also suggest using other psychometric instruments to reduce memory biases and broaden the understanding of the phenomena studied, such as assessing the woman's current perception of her parental bonds and the quality of the marital relationship. Thus, while the relationships between primary bonding and maternal-fetal attachment (MFA) have been explored, new studies should delve into the underlying mechanisms through which these relationships operate and are maintained (e.g., beliefs, schemas, adult attachment). It is important to emphasize that the results presented here should be interpreted in light of the specific characteristics of the sample and the collection site and are not generalizable to the entire population, as previously discussed based on the scientific literature.
REFERENCES
Altenburger, L. E. (2022). Similarities and differences between coparenting and parental gatekeeping: implications for father involvement research. Journal of Family Studies, 29(3), 1403-1427. https://doi.org/10.1080/13229400.2022.2051725 [ Links ]
Alves, T. O., Nunes, R. L. N., de Sena, L. H. A., Alves, F. G., de Souza, A. G. S., Salviano, A. M., Oliveira, B. R. D., Silva, D. I. de S., Lopes, L. M., Silva, V. D., de Almeida, L. P., Oliveira, R. D., de Jesus, E. C. P., Ruas, S. J. S., Santos, M. A., Pereira, Z. A. S., & Dias, J. L. C. (2021). Gestação de alto risco: epidemiologia e cuidados, uma revisão de literatura. Brazilian Journal of Health Review, 4(4), 14860-14872. https://doi.org/10.34119/bjhrv4n4-040 [ Links ]
Balle, R. E. (2017). Apego Materno-Fetal e Vínculos Parentais em Gestantes. (Dissertação de Mestrado, Universidade do Vale do Rio dos Sinos). Repositório Digital da Biblioteca da Unisinos. http://www.repositorio.jesuita.org.br/handle/UNISINOS/6832 [ Links ]
Baumrind, D. (1966). Effects of authoritative parental control on child behavior. Child Development, 37(4), 887-907. https://doi.org/10.2307/1126611 [ Links ]
Bhide, S., Sciberras, E., Anderson, V., Hazell, P., & Nicholson, J. M. (2019). Association between parenting style and socio-emotional and academic functioning in children with and without ADHD: A community-based study. Journal of Attention Disorders, 23(5), 463-474. https://doi.org/10.1177/1087054716661420 [ Links ]
Cabrera, N. J., Volling, B. L., & Barr, R. (2018). Fathers are parents, too! Widening the lens on parenting for children’s development. Child Development Perspectives, 12(3), 152-157. https://doi.org/10.1111/cdep.12275 [ Links ]
Campbell, C. G. (2022). Two decades of coparenting research: A scoping review. Marriage & Family Review, 59(6), 379-411. https://doi.org/10.1080/01494929.2022.2152520 [ Links ]
Çelik, F. P., & Güneri, S. E. (2020). The relationship between adaptation to pregnancy and prenatal attachment in high-risk pregnancies. Psychiatria Danubina, 32(Suppl 4), 568-575. https://pubmed.ncbi.nlm.nih.gov/33212465/ [ Links ]
Cerqueira, S. A., Reis, H. L., Nogueira, K. C., Coelho, T. J., & Manfroi, E. C. (2023). Apego materno-fetal em gestantes de alto risco: uma revisão integrativa. Psicologia Argumento, 41(115). https://doi.org/10.7213/psicolargum.41.115.AO14 [ Links ]
Cheraghi, P., & Jamshidimanesh, M. (2022). Relationship between maternal-fetal attachment with anxiety and demographic factors in high-risk pregnancy primipara women. Iran Journal of Nursing, 34(134), 46-59. https://doi.org/10.32598/ijn.34.6.4 [ Links ]
Cohen, J. (1992). Statistical power analysis. Current Directions in Psychological Science, 1(3), 98-101. https://doi.org/10.1111/1467-8721.ep10768783 [ Links ]
Cranley, M. S. (1981). Development of a tool for the measurement of maternal attachment during pregnancy. Nursing Research, 30(5), 281-284. https://doi.org/10.1097/00006199-198109000-00008 [ Links ]
Cuijlits, I., van de Wetering, A. P., Endendijk, J. J., van Baar, A. L., Potharst, E. S., & Pop, V. J. M. (2019). Risk and protective factors for pre- and postnatal bonding. Infant Mental Health Journal, 40(6), 768-785. https://doi.org/10.1002/imhj.21811 [ Links ]
Diniz, E., Brandão, T., Monteiro, L., & Veríssimo, M. (2021). Father involvement during early childhood: A systematic review of the literature. Journal of Family Theory & Review, 13(1), 77-99. https://doi.org/10.1111/jftr.12410 [ Links ]
Ferreira, C. I. M. (2016). Estilos Parentais e Qualidade de Vida em Crianças e Jovens (Dissertação de Mestrado, Escola Superior de Educação de Viseu). Repositório Científico do Instituto Politécnico de Viseu. http://hdl.handle.net/10400.19/4495 [ Links ]
Fraley, R. C., & Roisman, G. I. (2019). The development of adult attachment styles: four lessons. Current Opinion in Psychology, 25, 26-30. https://doi.org/10.1016/j.copsyc.2018.02.008 [ Links ]
Fukui, N., Motegi, T., Watanabe, Y., Hashijiri, K., Tsuboya, R., Ogawa, M., Sugai, T., Egawa, J., Enomoto, T., & Someya, T. (2021). Perceived parenting before adolescence and parity have direct and indirect effects via depression and anxiety on maternal-infant bonding in the perinatal period. Psychiatry and Clinical Neurosciences, 75(10), 312-317. https://doi.org/10.1111/pcn.13289 [ Links ]
Gadelha, I. P., Aquino, P. S., Balsells, M. M. D., Diniz, F. F., Pinheiro, A. K. B., Ribeiro, S. G., & Castro, R. C. M. B. (2020). Quality of life of high risk pregnant women during prenatal care. Revista Brasileira de Enfermagem, 73(Suppl 5), e20190595. https://doi.org/10.1590/0034-7167-2019-0595 [ Links ]
Gioia, M. C., Cerasa, A., Muggeo, V. M. R., Tonin, P., Cajiao, J., Aloi, A., Martino, I., Tenuta, F., Costabile, A., & Craig, F. (2023). The relationship between maternal-fetus attachment and perceived parental bonds in pregnant women: Considering a possible mediating role of psychological distress. Frontiers in Psychology, 13. https://doi.org/10.3389/fpsyg.2022.1095030 [ Links ]
Göbel, A., Barkmann, C., Arck, P., Hecher, K., Schulte-Markwort, M., Diemert, A., & Mudra, S. (2019). Couples' prenatal bonding to the fetus and the association with one's own and partner's emotional well-being and adult romantic attachment style. Midwifery, 79, 102549. https://doi.org/10.1016/j.midw.2019.102549 [ Links ]
Gomide, P. I. C. (2006). Inventário de Estilos Parentais. Modelo teórico: manual de aplicação, apuração e interpretação. Vozes. [ Links ]
Gonzalez, J., Klein, C., Barnett, M., Schatz, N., Garoosi, T., Chacko, A., & Fabiano, G. (2023). Intervention and implementation characteristics to enhance father engagement: A systematic review of parenting interventions. Clinical Child and Family Psychology Review, 26, 3. https://doi.org/10.1007/s10567-023-00430-x [ Links ]
Grossmann, K., Grossmann, K. E., Kindler, H., & Zimmermann, P. (2008). A wider view of attachment and exploration: The influence of mothers and fathers on the development of psychological security from infancy to young adulthood. Em J. Cassidy & P. R. Shaver (Eds.), Handbook of attachment: Theory, research, and clinical applications (2nd ed., pp. 857-879). The Guilford Press. [ Links ]
Handelzalts, J. E., Preis, H., Rosenbaum, M., Gozlan, M., & Benyamini, Y. (2018). Pregnant women’s recollections of early maternal bonding: Associations with maternal-fetal attachment and birth choices. Infant Mental Health Journal, 39(5), 511-521. https://doi.org/10.1002/imhj.21731 [ Links ]
Henry, J. B., Julion, W. A., Bounds, D. T., & Sumo, J. (2020). Fatherhood matters: An integrative review of fatherhood intervention research. The Journal of School Nursing, 36(1), 19-32. https://doi.org/10.1177/1059840519873380 [ Links ]
Hinesley, J., Amstadter, A., Sood, A., Perera, R. A., Ramus, R., & Kornstein, S. (2020). Adverse childhood experiences, maternal/fetal attachment, and maternal mental health. Women's Health Reports, 1(1), 550-555. https://doi.org/10.1089/whr.2020.0085 [ Links ]
Karantzas, G. C., Younan, R., & Pilkington, P. D. (2023). The associations between early maladaptive schemas and adult attachment styles: A meta-analysis. Clinical Psychology: Science and Practice, 30(1), 1-20. https://doi.org/10.1037/cps0000108 [ Links ]
Lima, C. de A., Brito, M. F. S. F., Pinho, L. de., Leão, G. M. M. S., Ruas, S. J. S., & Silveira, M. F. (2022). Abbreviated version of the Maternal-Fetal Attachment Scale: Evidence of validity and reliability. Paidéia (Ribeirão Preto), 32, e3233. https://doi.org/10.1590/1982-4327e3233 [ Links ]
Lucena, A. da S., Ottati, F., & Cunha, F. A. (2019). O apego materno-fetal nos diferentes trimestres da gestação. Psicologia para América Latina, 31, 13-24. [ Links ]
Maccoby, E. E., & Martin, J. A. (1983). Socialization in the Context of the Family: Parent-Child Interaction. In P. H. Mussen, & E. M. Hetherington (Eds.), Handbook of Child Psychology: Vol. 4. Socialization, Personality, and Social Development (pp. 1-101). Wiley. [ Links ]
Martins, R. P. M. P., Nunes, S. A. N., Faraco, A. M. X., Manfroi, E. C., Vieira, M. L., & Rubin, K. H. (2014). Práticas parentais: associações com desempenho escolar e habilidades sociais. Psicologia Argumento, 32(78). https://doi.org/10.7213/psicol.argum.32.078.AO04 [ Links ]
McNamara, J., Townsend, M. L., & Herbert, J. S. (2019). A systemic review of maternal wellbeing and its relationship with maternal fetal attachment and early postpartum bonding. PloS one, 14(7), e0220032. https://doi.org/10.1371/journal.pone.0220032 [ Links ]
Ministério da Saúde. (2016). Guia do Pré-Natal do Parceiro para Profissionais de Saúde. Brasil. Secretaria de Atenção à Saúde, Departamento de Ações Programáticas Estratégicas, Coordenação Nacional de Saúde do Homem. https://bvsms.saude.gov.br/bvs/publicacoes/guia_pre_natal_parceiro_profissionais_saude.pdf [ Links ]
Mourão, L., Ferreira, M. C., & Martins, L. F. (2021). Regressão múltipla linear. Em C. Faiad, M. N. Baptista, & R. Primi (Orgs.), Tutoriais em análises de dados aplicados à psicometria (pp. 102-127). Vozes. [ Links ]
Nascimento, V. M. S., Reis, H. L., & Manfroi, E. C. (2022). Promovendo práticas parentais positivas: avaliação de um modelo interventivo online para pais de adolescentes. Psicologia Argumento, 40(111). https://doi.org/10.7213/psicolargum.40.111.AO07 [ Links ]
Papalia, D. E., & Martorell, G. (2022). Desenvolvimento humano (14th ed.). AMGH. [ Links ]
Parker, G., Tupling, H., & Brown, L. B. (1979). A Parental Bonding Instrument. British Journal of Medical Psychology, 52(1), 1-10. https://doi.org/10.1111/j.2044-8341.1979.tb02487.x [ Links ]
Ponti, L., Smorti, M., Ghinassi, S., & Tani, F. (2021). The relationship between romantic and prenatal maternal attachment: The moderating role of social support. International Journal of Psychology, 56(1), 143-150. https://doi.org/10.1002/ijop.12676 [ Links ]
Provenzi, L., Brambilla, M., Scotto di Minico, G., Montirosso, R., & Borgatti, R. (2020). Maternal caregiving and DNA methylation in human infants and children: Systematic review. Genes, Brain, and Behavior, 19(3), e12616. https://doi.org/10.1111/gbb.12616 [ Links ]
Reed, O. (2014). The effect of maternal factors on prenatal attachment (Tese de honra de graduação, University of Redlands). Institutional Scholarly Publication and Information Repository. https://core.ac.uk/download/pdf/217141226.pdf [ Links ]
Richter, M., Schlegel, K., Thomas, P., & Troche, S. J. (2022). Adult attachment and personality as predictors of jealousy in romantic relationships. Frontiers in Psychology, 13, 861481. https://doi.org/10.3389/fpsyg.2022.861481 [ Links ]
Richter, P. do C., Ghedin, D. A. M., & Marin, A. H. (2018). “Por que meu filho reprova?” Estudo sobre o vínculo parental e a reprovação escolar. Educação, 43(3), 499-520. https://doi.org/10.5902/1984644423703 [ Links ]
Rocha, A. C., Reis, H. L., Sampaio, M. L., & Manfroi, E. C. (2022). O estar em UTI neonatal: percepções dos pais sobre a vivência da hospitalização e a assistência psicológica recebida na unidade. Contextos Clínicos, 15(3). https://doi.org/10.4013/ctc.2022.153.05 [ Links ]
Rodrigues, A. R. M., Dantas, S. L. C., Pereira, A. M. M., Silveira, M. A. M., & Rodrigues, D. P. (2017). Gravidez de alto risco: análise dos determinantes de saúde. SANARE-Revista de Políticas Públicas, 16, 23-28. [ Links ]
Rollè, L., Giordano, M., Santoniccolo, F., & Trombetta, T. (2020). Prenatal attachment and perinatal depression: A systematic review. International Journal of Environmental Research and Public Health, 17(8), 2644. https://doi.org/10.3390/ijerph17082644 [ Links ]
Rosa, K. M., Scholl, C. C., Ferreira, L. A., Trettim, J. P., da Cunha, G. K., Rubin, B. B., Martins, R. D. L., Motta, J. V. D. S., Fogaça, T. B., Ghisleni, G., Pinheiro, K. A. T., Pinheiro, R. T., Quevedo, L. A., & de Matos, M. B. (2021). Maternal-fetal attachment and perceived parental bonds of pregnant women. Early Human Development, 154, 105310. https://doi.org/10.1016/j.earlhumdev.2021.105310 [ Links ]
Sacchi, C., Miscioscia, M., Visentin, S., & Simonelli, A. (2021). Maternal-fetal attachment in pregnant Italian women: Multidimensional influences and the association with maternal caregiving in the infant’s first year of life. BMC Pregnancy and Childbirth, 21(1), 488. https://doi.org/10.1186/s12884-021-03964-6 [ Links ]
Santana, C. V. N., & Souza, R. P (2018). Epigenética e desenvolvimento humano. Em D. M. Miranda & L. F. Malloy Diniz (Eds.), O pré-escolar (3rd ed., pp. 23-31). Hogrefe. [ Links ]
Schmidt, E. M., Décieux, F., Zartler, U., & Schnor, C. (2023). What makes a good mother? Two decades of research reflecting social norms of motherhood. Journal of Family Theory & Review, 15(1), 57-77. https://doi.org/10.1111/jftr.12488 [ Links ]
Selcuk, E., Ascigil, E., & Gunaydin, G. (2024). A theoretical analysis and empirical agenda for understanding the socioecology of adult attachment. European Review of Social Psychology, 1-34. https://doi.org/10.1080/10463283.2024.2367894 [ Links ]
Soares, B., Vivian, A. G. V., & Sommer, J. A. P. (2022). Apego materno-fetal, ansiedade e depressão na gestação de alto risco. Concilium, 22(2), 36-49. https://doi.org/10.53660/CLM-086-108 [ Links ]
Suryaningsih, E. K., Gau, M. L., & Wantonoro, W. (2020). Concept analysis of maternal-fetal attachment. Belitung Nursing Journal, 6(5), 157-164. https://doi.org/10.33546/bnj.1194 [ Links ]
Teixeira, M., Raimundo, F., & Antunes, C. (2016). Relation between maternal-fetal attachment and gestational age and parental memories. Revista de Enfermagem Referência, IV Série, 85-92. https://doi.org/10.12707/RIV15025 [ Links ]
Teodoro, M. L. M., Benetti, S. P. da C., Schwartz, C. B., & Mônego, B. G. (2010). Propriedades psicométricas do Parental Bonding Instrument e associação com funcionamento familiar. Avaliação Psicológica, 9(2), 243-251. [ Links ]
Topan, A., Kuzlu Ayyıldız, T., Sahin, D., Kilci Erciyas, Ş., & Gultekin, F. (2022). Evaluation of mother-infant bonding status of high-risk pregnant women and related factors. Clinical and Experimental Health Sciences, 12(1), 26-31. https://doi.org/10.33808/clinexphealthsci.766888 [ Links ]
Trombetta, T., Giordano, M., Santoniccolo, F., Vismara, L., Della Vedova, A. M., & Rollè, L. (2021). Prenatal attachment and parent-to-infant attachment: A systematic review. Frontiers in Psychology, 12, 620942. https://doi.org/10.3389/fpsyg.2021.620942 [ Links ]
van Bussel, J. C., Spitz, B., & Demyttenaere, K. (2010). Reliability and validity of the Dutch version of the maternal antenatal attachment scale. Archives of Women's Mental Health, 13(3), 267-277. https://doi.org/10.1007/s00737-009-0127-9 [ Links ]
Vieira, A. F., & Aguiar, R. S. (2021). Benefícios para a gestante com a participação paterna no pré-natal: Uma revisão integrativa. Saúde Coletiva (Barueri) , 11(68), 7375-7386. https://doi.org/10.36489/saudecoletiva.2021v11i68p7375-7386 [ Links ]
Weber, L. N. D. (2017). Relações entre práticas educativas parentais percebidas e a autoestima, sinais de depressão e o uso de substâncias por adolescentes. Revista INFAD de Psicología. International Journal of Developmental and Educational Psychology, 2(1), 157-168. https://doi.org/10.17060/ijodaep.2017.n1.v2.928 [ Links ]
Wendt, G. W., & Appel-Silva, M. (2020). Práticas parentais e associações com autoestima e depressão em adolescentes. Pensando famílias, 24(1), 224-238. [ Links ]
Yarcheski, A., Mahon, N. E., Yarcheski, T. J., Hanks, M. M., & Cannella, B. L. (2009). A meta-analytic study of predictors of maternal-fetal attachment. International Journal of Nursing Studies, 46(5), 708-715. https://doi.org/10.1016/j.ijnurstu.2008.10.013 [ Links ]
How to cite: Lima Reis, H., Cardoso Nogueira, K., Manfroi, E. C., & Pereira Gonçalves, A. (2024). Perceived parental bonding and variables associated with maternal-fetal attachment in high-risk pregnancy. Ciencias Psicológicas, 18(2), e-3598. https://doi.org/10.22235/cp.v18i2.3598
Authors’ contribution (CRediT Taxonomy): 1. Conceptualization; 2. Data curation; 3. Formal Analysis; 4. Funding acquisition; 5. Investigation; 6. Methodology; 7. Project administration; 8. Resources; 9. Software; 10. Supervision; 11. Validation; 12. Visualization; 13. Writing: original draft; 14. Writing: review & editing. H. L. R. has contributed in 1, 2, 3, 4, 5, 6, 7, 8, 10, 11, 12, 13, 14; K. C. N. in 1, 5, 6, 7, 8, 9, 13, 14; E. C. M. in 1, 3, 4, 6, 7, 8, 10, 12, 14; A. P. G. in 2, 3, 6, 9, 11, 12, 13, 14
Received: July 26, 2023; Accepted: September 23, 2024











 texto en
texto en