Demographic aging is one of the most significant transformations of our time. The older people population in 2021 was slightly superior to one billion, corresponding to nearly 13.5% of the world population. Estimations state that by 2030, one out of every six people will be 60 years or older (World Health Organization, 2021). In Mexico, the proportion of older people is rapidly increasing. In 2020, 15.1 million 60-year-old people and older resided in Mexico, representing 12% of the total population (Instituto Nacional de Estadística y Geografía, 2021).
Unfortunately, aging is frequently associated with chronic diseases, including dementia and cognitive impairment. The prevalence of dementia is 7.9%, and 7.3% for mild cognitive impairment (MCI) in the Mexican population. For both conditions, the frequency is higher in women, older-age participants, people with less schooling, and rural area residents. Other studies highlight that hypertension, diabetes, sensory impairment, and depression are risk factors for dementia but not for MCI (Mejía-Arango et al., 2020). MCI could represent an early stage of Dementia; it is characterized by the decline in the expected cognitive function regarding age and schooling level and is used to refer to a low-level neurocognitive affectation. In some cases or more severe conditions, it is linked to pathological processes associated with the presence or not of dementia. However, both are essential factors for functional dependency (Ataollahi Eshkoor, Mun, Ng y Hamid, 2015).
Diverse social and psychological variables, particularly mental health, are crucial for a healthy aging process. Reported data show a positive association between cognitive impairment and social support networks, marital status, and social participation (Zunzunegui, Alvarado, Del Ser y Otero, 2003). Also, some antecedents reflect the importance of the correlation between some psychological conditions like depressive symptoms, low income, participation in social activities, and social support networks with cognitive impairment (Song, Yu, Li, He y Sun, 2019).
Foong et al. reported that the relationship between psychosocial stress (measured by perceived stress, depression, loneliness, and neuroticism); and global cognition (calculated by MMSE and MOCA) was found to be significant in men only. The reason could be that psycho-social stress and depression are associated with dopaminergic dysfunction and structural changes in the brain (Foong, Hamid, Ibrahim y Haron, 2018).
However, to our knowledge, there needs to be reported evidence about the simultaneous evaluation of various psychological and social variables that could be associated with cognitive function scores.
Therefore, this article aims to study the relationship between ten psycho-social features (depressive symptoms, volunteering, perception of loneliness, internal locus of control, attendance to religious services, personal decision-making, socioeconomic status perception, life satisfaction, perception of health, and active participation in working life) and the cognitive function of adults and older people in Mexico.
Materials and Methods
We considered the population surveyed in the 2018 round of the National Study of Ageing and Health in Mexico (MHAS for its acronym in English). The MHAS is a longitudinal study on the 50-year-old and older population. The baseline survey, with national and urban/rural representation of adults born in 1951 or earlier, was conducted in 2001 with five follow-up waves until the present report. The aim, design, methodological aspects, sample frame, sample process, and sample size of the MHAS have been previously published and are widely explained on the study's webpage (Wong, Michaels-Obregon y Palloni, 2017).
The MHAS consists of five survey rounds; the first round, 2001, had a basal sample of 15,402 participants. The round in 2003 studied 14,386 participants. A further round in 2012 comprised 18,465 participants, which included 5,896 new participants. In 2015, 15,898 participants were surveyed. The total number of deaths rose to 4,491 in 2015.
The 2018 survey comprised 18,248 participants, of which 15,786 were face-to-face interviews. The sample was refreshed in this round, and approximately 4,500 participants between 50 and 55 were added (Instituto Nacional de Estadística y Geografía, 2018).
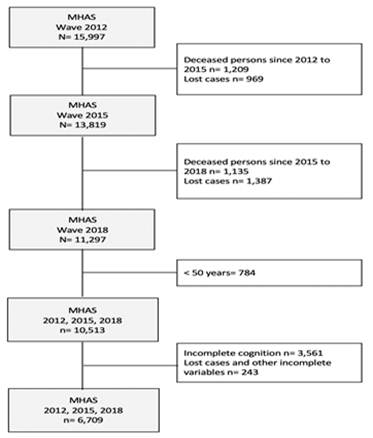
The present study is based on the fifth round (2018) analysis and is part of a longitudinal analysis, for which wave pasting 2012, 2015, and 2018 were performed. Only participants reported in the three waves were analyzed. After eliminating deceased participants, lost cases, and persons under 50 years, the rounds showed 11,297. We selected those participants who, in the 2018 round, entirely answered the socio-demographic, psycho-social, functional, and multi-morbidity variables and who concluded the cognitive sections: verbal learning, verbal learning evocation, visuospatial skills, visual memory, visual scanning, orientation, and verbal fluency. Finally, the sample was composed of 6,709 participants (Figure 1).
Measurements
A set of questionnaires (socio-demographic, health, cognition, functional status, among others) was applied face-to-face by trained interviewers.
Dependent variable
The MHAS includes the Cross-Cultural Cognitive Examination (CCCE) instrument to evaluate cognition.
All the included tasks in the CCCE are accepted as cognitive function indicators, being a trusted, reliable, and sensitive tool for the diagnosis of dementia in the population (Díaz-Venegas, Samper-Ternent, Michaels-Obregón y Wong, 2019; Glosser et al., 1993).
The scales applied in the 2018 round were: verbal learning (0-8 points), verbal learning evocation (0-8 points), visuospatial skills (0-6 points), visual memory (0-6 points), visual scanning (0-60 points), orientation (0-3 points) and verbal fluency (1-4 points). The score in every scale is summed, and the total was standardized, as expected; the mean must be 0 and the standard deviation of 1. The maximum possible value is 95 points. The higher scores represent a better cognitive function (Mejía Arango, Wong y Michaels-Obregón 2015).
Independent variables
Depressive symptoms were measured using the Yesavage geriatric depression scale (EDG), which consists of 9 questions:
Have you felt depressed?, Have you felt that everything you did was an effort? Have you felt that your sleep is restless?, Have you felt happy? Have you felt lonely? Have you felt that you enjoyed life? Have you felt sad?, Have you felt tired? (and) Have you felt you used to have much energy?.
The two positive items were reversed for calculating the total score. The cut-off point was to have more than five answers positive to depressive symptoms (Aguilar-Navarro, Fuentes-Cantú, Ávila-Funes y García-Mayo, 2007).
The volunteering aspect was assessed through two questions: have you volunteered for educative-religious organizations, charity, or for the community? and did you volunteer or support any civil organization without receiving payment or compensation? (Yes/No).
To examine the perception of loneliness, the UCLA Loneliness Scale was used, and a variable was created using three questions: Do you feel you lack company? Do you feel ignored by others? Do you feel isolated or away from others? An index of loneliness was constructed where the minimum value is three and the maximum is nine; the higher the number, the higher the feeling of loneliness perceived by the subject (Rusell, Peplau, y Cutrona, 1980).
The internal locus of control was assessed with the statements:
Every person is responsible for his or her own success, You can do almost anything you set out to do, Our misfortunes are the result of our own mistakes, (and) Every person is responsible for his or her own failures.
Scores being from 1 = agree, 2 = slightly agree, 3 = slightly disagree to 4 = disagree (Rotter, 1966). On a global score, four indicates an adequate internal locus of control, and 16 indicates a low internal locus of control.
Concerning the attendance to religious practices variable, the question was: do you attend religious practices regularly? (Yes/No).
To measure personal decision-making the question was: when you face an important personal decision like going to the doctor or having surgery, how much are you responsible for the final decision? This was a dichotomous variable (a lot = high personal decision-making/a little or none = low personal decision-making).
To assess the perception of economic status, the question was: would you say that your economic status is …? This was a dichotomous variable: average or low = low perception of economic status, and excellent / very good / good = high perception of economic status.
In regards to overall satisfaction in life, the statements were:
My life is close to ideal in most things, My life conditions are excellent, I am satisfied with my life, So far, I have achieved what is important in life, If I were born again (and) I would not change anything about my life.
This was also a dichotomous variable: agree = very satisfied with life, neither agree nor disagree/disagree = less satisfied with life or not at all.
For health perception, two main categories were analyzed: excellent/very good/good = good, and regular/bad = bad, as described in previous research (Haseen, Adhikari y Soonthorndhada, 2010).
In the case of working life, the question was: are you currently employed? Yes = employed or No = in search of employment or unemployed.
Confounding variables
Socio-demographic characteristics were also analyzed (gender, age, years of schooling, marital status), multi-morbidity, and functionality. Also access to health services was also included.
For multi-morbidity, the presence or absence of the following pathologies was evaluated by self-report: diabetes mellitus, arterial hypertension, brain stroke, fall syndrome, heart stroke, pulmonary disease, cancer, and arthritis. Also, we included if participant uses a hearing aid. For the perception of sleep quality, the following question was asked: how often do you feel tired when you wake up in the morning? Most of the time/Sometimes = bad sleep quality, Rarely/Never = good sleep quality.
Consumption of alcohol was measured with the question do you currently drink alcoholic beverages such as beer, wine, liquor, or pulque? (Yes/No). Smoking habits throughout life were analyzed with two questions: Have you ever smoked cigarettes? (Yes/No) and in the last two years: did you smoke cigarettes (Yes/No)? For functionality, the survey included five out of six activities considered from the Katz index: using the toilet, difficulty walking, feeding oneself, going to bed, and bathing oneself. The activities were considered dichotomous variables, asking whether the subject is capable or needs help performing each activity mentioned above (Dorantes-Mendoza, Ávila-Funes, Mejía-Arango y Gutiérrez-Robledo, 2007; Katz, 1963).
Statistical methods
Descriptive analyses were performed on the sample to obtain distribution percentages and mean for each variable according to the variable type, globally, and by gender.
Bivariate analyses between the inputs (independent and confounders) and response variables by sex and globally were performed according to the variable type. In the case of binary variables, a t-test was used. In the case of qualitative variables (categorical and ordinal variables) with three or more groups, an ANOVA test was used. And in the case of quantitative variables, the association was measured using a Pearson correlation. It was verified graphically that the response variable has an approximately normal distribution associated with it.
To analyze the effect of psychosocial characteristics (independent variables) on cognition (dependent variable), a multiple linear regression was fitted by the socioeconomic, social, personality characteristics, and multi-morbidity measures. All model assumptions were verified through residuals, graphically and through tests.
Multicollinearity was analyzed through the variance inflation factor (VIF). The significance level used in all analyses was <0.05; all the analyses were performed in Stata Version 14.1.
According to the Declaration of Helsinki, the present study was adapted to the ethical and scientific principles in medical research on humans (Wong et al., 2017). The research was registered at the National Institute of Geriatrics under the registration number DI-PI-006/2022.
Results
From the sample included in the study (n= 6,709), 41.1 % (n=2,761) were men, and 58.8% (n=3,948) were women. The average age was 68.2 years old. The middle schooling for the total participants was 6.2 years. Other sociodemographic characteristics can be seen in Table 1.
Table 1: Sociodemographic characteristics of the study sample by sex
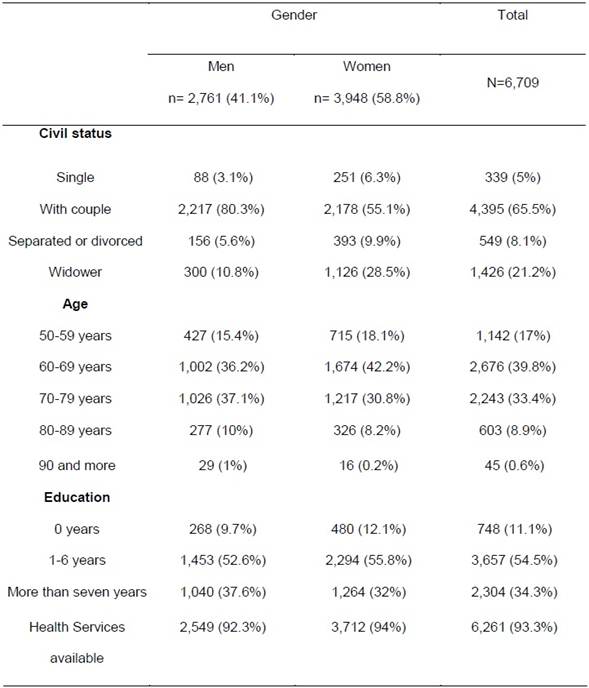
Note: Compilation based on the ENASEM 2018.
About the independent variables, participants with depressive symptoms were 28% (n=1,879), and 23.1% were involved in volunteering. In the perception of loneliness, the mean value for women was 4.04, and for men was 3.73. In the case of the internal locus of control, the mean value for men was 5.02, and for women. Comparing the mean values of standardized cognition score, we found some significant differences for both sexes in depressive symptoms (p<0.001), volunteer work (p<0.001), and making decisions independently (p<0.001), good socioeconomic perception (p<0.001), and poor perception of health (p<0.001). Perception of loneliness was also found significant (p<0.001). Surprisingly, attendance at religious services (p<0.001), satisfaction in life health (p<0.001), and currently employed (p<0.001), were also significant but negative scores were found to the positive answer of these three variables (Table 2).
Table 2: Bivariate analysis between the independent psychosocial variables and the dependent variable (cognition score), by sex, for all the individues. Mean or correlation index are included for each variable and by sex
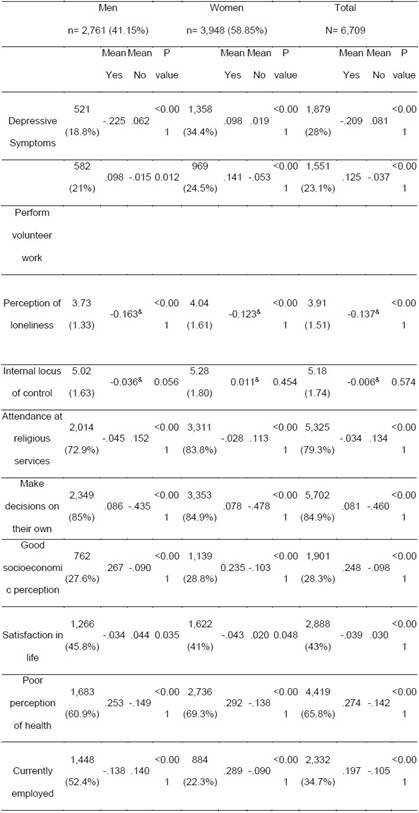
Note: Compilation based on the ENASEM 2018. yPearson correlation index. t-test in the rest of variables, *Scale 3-9; 3 less perception of loneliness; 9 increased perception of loneliness. **Scale 4-16, 4 adequate locus of control, 16 low locus of control
Participants that self-reported arterial hypertension were 49.81% (n=3,342); 27.3% (n=1,1836) self-reported diabetes mellitus; 2% (n=136) reported having had brain stroke once. 43.3% (n=2,910) reported having fallen in the previous two years, 4.4% (n=297) reported having had a heart attack. Regarding smoking, 61.1% (n=4,099) reported they never smoked, 26.4% (n=26.4) said that they smoked before but do not smoke anymore, and 12.4% (n=836) reported having smoked and also they currently smoke. Active alcohol consumption is reported by 25.8% (n= 1,735), 2.8% (n= 194) of the participants responded having a history of cancer, 6.3% (n= 426) suffer pulmonary disease, 13.7% (n=919) are diagnosed with rheumatoid arthritis. 2.2% (n=150) use a hearing aid, and 85.3% (n=5,726) referred suffering from bad sleep quality. Bivariate analysis is presented in Table 3. Hypertension, diabetes, stroke, falls, pulmonary diseases, and arthritis were found with significant mean differences in the score of cognition in the total sample, with some differences among men and women (Table 3).
Table 3 Bivariate analysis between multi-morbidity by sex and cognition.
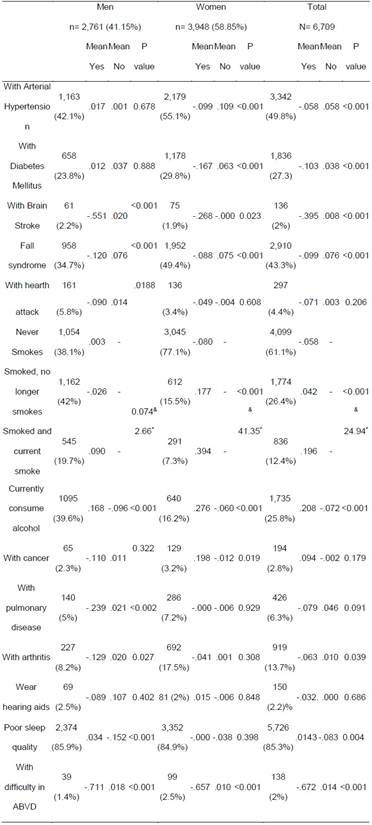
Note: Compilation based on the ENASEM 2018. yOneway index. *Value F Oneway
Linear regression
The model was adjusted to the following variables: age, gender, civil status, socio-economic status perception, schooling, arterial hypertension, diabetes mellitus, brain embolism, falls, heart stroke, smoking, alcohol consumption, cancer history, pulmonary disease, rheumatoid arthritis, hearing aid, poor sleep quality, access to health services, and daily-life activities. The linear regression model shows a p-value of 0.000, associated with the F test; therefore, we can conclude that the variables are jointly related to cognitive scoring (Table 4). It was determined that there was no multicollinearity (VIF= 1.55). Results revealed that being a woman predicts better cognitive function (β=.117, CI 95% .069, .165 p=0.000). Participants with higher schooling have a better cognitive function (β=1.27, CI 95% 1.20, 1.34 p<0.001), and those who are older have a minor cognitive function (β=-1.30, CI 95% -1.54, -1.06 p<0.001).
Table 4: Linear regression coefficients.
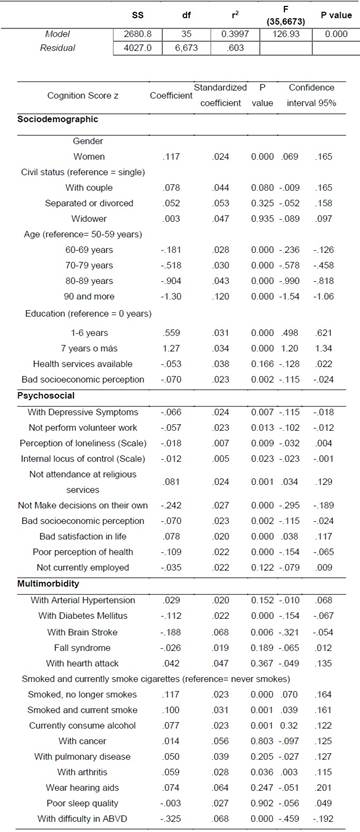
Note: Compilation based on the ENASEM 2018. F-value=126.93 (35/6673), p-value= 0.000 , y r2= 0.399
Participants with depressive symptoms (β=-.066, CI 95% -.115, -.018 p=0.007) or reported null activity in volunteering (β=-.057, CI 95% -.102, -.102 p=0.013), with feelings of loneliness (β=--.018, CI 95% -.032, .004 p=0.009), and those who mentioned having a poor perception of health (β=-.109, CI 95% -.154, -.065 p<0.001), showed lower cognitive scoring. Regarding the participants with a low internal locus of control (β=-.012., CI 95% -.023, -.001 p=0.023), the cognition score declined, as well as those who answered not being involved in personal decision-making (β=-.242, CI 95% -.295 , -.189 p<0.001), and those reporting lower economic-status perception (β=-.070., CI 95% -.115, -.024 p=0.002). Finding themselves indifferent or unsatisfied with life perception (β=.078., CI 95% .038, .117 p=0.000) and reported no attendance to religious services perception (β=.081., CI 95% .034, .129 p=0.001), cognitive score remained the same.
The cognition score was lower for participants suffering from diabetes (β=.112, CI 95% -.154, -.067 p<0.001), those who reported having had a stroke (β=-.188., CI 95% -.321, -.054 p=0.006), and those who experimented with difficulties in basic everyday activities (β=-.325., CI 95% -.459, -.192 p<0.001). For those participants reporting active alcohol consumption (β=.077., CI 95% 0.32, .122 p=0.001), smoking history, those who smoked and currently smoke (β=.100, CI 95% .039, .161 p=0.001), and rheumatoid arthritis diagnosis (β=.059., CI 95% .003, .115 p=0.036), the cognitive development score was better.
Discussion
The results indicate that being a woman predicts a better cognitive function for older adults, as well as having higher schooling and being younger compared to older participants. This research also revealed data about decreasing cognition scores concerning some psycho-social characteristics such as depression, not volunteering, feelings of loneliness, low internal locus of control, lack of personal decision-making, and low economic-status perception, fostering the relationship between psycho-social characteristics and cognition level.
The process of aging is determined by various factors, such as genetic and environmental factors; during this process, the human body faces numerous changes: physical, social, emotional, economic, cultural, and social, which may impact the aging process (Aliaga-Díaz, Cuba-Fuentes y Mar-Meza, 2016). Thus, the purpose of this study has been to understand the connection between the psychological and social characteristics and the cognitive development of older people in México.
Just like literature has described the impact of aging on cognitive performance, other factors have also been reported to show additional precedents that may impact cognitive functions. A study of the Mexican population showed a greater chance for women to manifest cognitive impairment (Mejía-Arango, Miguel-Jaimes, Villa, Ruiz-Arergui y Gutiérrez-Robledo, 2007). In another study conducted over the MHAS population on 2001 and 2012 rounds, Díaz-Venegas et al. (2019) reported a significant reduction in gender disparity in cognition among older people; it is expected that, as women reach a higher schooling level, the gender gap in cognition among future cohorts of Mexican older people will be reduced. This effect can be evident in the present cohort since it was found that women showed better cognitive performance than men.
The effect of years of schooling has been studied on cognitive performance about the age of older people. In a Lenehan et al., review, it was concluded that little evidence supports the theory that years of schooling moderate cognitive performance related to the age of healthy older people (Lenehan, Summers, Saunders, Summers y Vickers, 2015). This study showed that participants with higher education (7 years and above) presented a better cognitive performance, concerning older people with no schooling and those with 1 to 6 years of education.
Schooling may impact older people’s cognitive performance from the perspective of cognitive reserve; it could also help in other aspects, such as friendships and better social support networks. Therefore, including psycho-social evaluation in the aging process is substantial, specifically in older people’s cognitive deterioration (Foong et al., 2018). As we can see in this research, psycho-social factors might impact cognition scores negatively.
The aging process involves various physical, psychological, emotional, social, and economic changes, representing the probability of manifesting a vulnerable condition coupled with specific pathologies. Changes in economic status, access to health services, loss, and bereavement in old age are some stressors and impact factors at this life stage. Therefore, it is essential to consider the multifactorial factors that affect the individual’s aging in their community to analyze older people’s performance in cognitive functions. In a study conducted by Segura Cardona, Garzón Duque, Cardona Arango y Segura Cardona (2016) (in which it was sought to know the prevalence of risk of mental deterioration and its relationship with demographic, social, and functional factors), it was found that older people, without a partner, a lower schooling, scarce social resources, not attending community groups, having a poor perception of life quality, being dissatisfied with health, and functionally dependent for basic activities were at higher risk of cognitive impairment (Segura Cardona et al., 2016). The literature has described that in order to achieve successful aging, positive social relationships and good health have been considered to be two important determinants of successful aging (Ha, Kahng y Choi 2017); this study showed that people who reported not volunteering, feeling lonely, not participating in important decisions, and those with a low internal locus of control had poorer cognitive performance.
The results in the present research showed that the participants who reported being indifferent or unsatisfied with life and those who did not attend religious services scored a higher cognitive performance, opposite of participants who actively participated in religious services and reported overall satisfaction with life. A possible hypothesis for these controversial findings could be related to a different worldview, less optimistic and, at the same time, more critical. It may reflect a higher level of intellectuality. Indeed, these ideas have to be further studied.
According to the analyzed data for this research, the results showed that participants with depressive symptoms had a lower score in cognitive functions; this matches what is stated in the literature, where it is clear that depression is one of the risk factors associated with cognitive impairment (Rentería et al., 2020). For participants reporting a bad economic situation, the scoring for cognitive functions was also lower, which might be linked with the participants’ emotional state.
Social networks and social integration are essential factors in determining older people’s social links, as analyzed in a study by Zunzunegui et al. (2003), where the authors concluded that scarce social connections and infrequent participation in social activities predict cognitive impairment in older people. It is crucial to analyze the older adult from our cultural standpoint, history, and beliefs from past and present decades; according to Jeon, Jang, Kim y Cho (2013), in the research on the Korean population, culture, family manners, and family beliefs play a fundamental role in older people’s aging, since they will have better social connections to support them when aging.
Some interesting data in the participants’ answers showed that participants who actively consume alcoholic beverages showed higher cognitive functioning. Although, a limitation of the study is that the motivation for the participant’s alcohol consumption is unknown. It has been reported that in the older adult population, one of the motivations for alcohol consumption is social coexistence, as described by Gilson et al. (2013) in a study, where it is clarified that the social motivations for alcohol consumption were the most frequent, followed by psychological reasons, such as improvement, and coping.
Study limitations that are relevant to mention are the following: some participants were discarded for having incomplete answers on the cognitive scale. It is impossible to recognize whether people who refuse to answer might have a cognitive impairment, and therefore, there is some probability of underestimating the effect. However, the simple size shows an acceptable level of significance.
People age under different cultures, beliefs, families, and social structures that can impact life history and therefore affect the course of diseases. Bearing this in mind, variables that were significant in this research, such as participating in social activities and personal decision-making, are of interest to making better decisions to improve older people’s cognitive health processes (Song et al., 2019). Therefore, it is vital to consider the quality and quantity of social resources and the psychological characteristics within the analysis of older people’s cognitive functions as modifiable factors that could negatively impact the diagnosis of cognitive impairment.
Conclusions
According to the results, cognition is significantly affected in the group of men, in people with higher age, with less schooling, for people with depressive symptoms, those who do not perform any volunteer service, for participants who do not participate in decision-making, those with a low internal locus of control, those with poor economic perception. The present study reveals the importance of evaluating psychosocial factors in older persons since these factors can have an important effect in cognition and because some of these variables are modifiable, such as depression or loneliness, health and social services can prevent or at least delay negative cognitive impacts.
Funding
The MHAS (Mexican Health and Aging Study) is partly sponsored by the National Institutes of Health/National Institute on Aging (grant number NIH R01AG018016) in the United States and the Instituto Nacional de Estadística y Geografía (INEGI) in Mexico.
Acknowledgments
The authors thanks the Mexican National Council of Humanities, Sciences and Technologies (CONAHCYT, acronym in Spanish) for the graduate scholarship of M.A. Barragán-García (CVU: 779814), who is a student of the Master´s and Doctoral Program in Medical, Dental and Health Sciences of national Autonomous University of Mexico (UNAM, acronym in Spanish).
Institutional Review Board Statement
The current analysis was registered at the National Institute of Geriatrics under the registration number DI-PI-006/2022. The MHAS was approved by the Institutional Review Boards and Ethics Committees of the University of Texas Medical Branch in the USA, the Instituto Nacional de Estadística y Geografía (INEGI), and the Instituto Nacional de Salud Pública (INSP) in Mexico.